Submitted:
11 December 2025
Posted:
12 December 2025
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Collection
2.2. Toxicological Analysis
2.3. Geospatial Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BAC | Blood alcohol concentration |
| DPR | Drug problem ratio |
| HDI | Human development index |
| OR | Odds ratio |
| PSA | Psychoactive substances |
| THC | Δ9-tetrahydrocannabinol |
References
- World Health Organization – WHO. Global health estimates: Leading causes of death. Cause-specific mortality, 2000-2021, 2022. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. (accessed on 03/12/2024).
- Brazil, Ministry of Health. External causes mortality data. Available online: https://datasus.saude.gov.br/mortalidade-desde-1996-pela-cid-10. (accessed on 25/11/2025).
- Pan American Health Organization – PAHO. Leading causes of mortality and health loss at regional, subregional, and country levels in the Region of the Americas, 2000-2019. Available online: https://www.paho.org/en/enlace/leading-causes-death-and-disability. (accessed on 03/12/2025).
- Goldstein, P.J. The drugs/violence nexus: a tripartite conceptual framework. J Drug Issues 1985, 15(4), 493-506. [CrossRef]
- Guimarães, R.A.; Mesquita, N.S.; Lopes, R.S; Lucchese, R.; de Felipe, R.L.;Vera, I; Fernandes, I.L.; de Castro, P.A.; Monteiro, L.H.B.; Silva, G.C. Prevalence and Factors Associated with Criminal Behavior Among Illicit Drug Users: A Cross-Sectional Study. Subst Use Misuse 2017, 52(11), 1393-1399. [CrossRef]
- Centro de Excelência para a Redução da Oferta de Drogas Ilícitas – CdE. Dinâmicas do mercado de drogas ilícitas no Brasil. Análise comparativa dos preços de maconha, cocaína e outras drogas em quatro estados. Available online: https://cdesc.org.br/publicacoes/. (accessed on 25/11/2025).
- Andreuccetti, A.; Cherpitel, C.J.; Carvalho, H.B.; Leyton, V.; Miziara, I.; Muñoz, D.R.; Reingold, A.L.; Lemos, N.P. Alcohol in combination with illicit drugs among fatal injuries in Sao Paulo, Brazil: An epidemiological study on the association between acute substance use and injury. Injury 2018, 49, 2186-2192. [CrossRef]
- Auckloo, M.B.K.M.; Davies, B.B. Post-mortem toxicology in violent fatalities in Cape Town, South Africa: A preliminary investigation. J Forensic Leg Med 2019, 63, 18-25. [CrossRef]
- Darke, S.; Duflou, J. Toxicology and circumstances of death of homicide victims in New South Wales, Australia 1996-2005. J Forensic Sci 2008, 53(2), 447-451. [CrossRef]
- Di Candia, D.; Giordano, G.; Boracchi, M.; Zoja, R. Postmortem forensic toxicology cases: A retrospective review from Milan, Italy. J Forensic Sci 2022, 67(4), 1640-1650. [CrossRef]
- De Holanda Júnior, W.P.; Maceno, R.H.M.; Ferreira, M.A.D. Fatores sociodemográficos de mortes violentas relacionadas a substâncias psicoativas lícitas ou ilícitas: estudo transversal, Ceará, 2015-2019. RESS 2024, 33:e2024152. [CrossRef]
- Lemos, Y.V.; Wainstein, A.J.A.; Savoi, L.M.; Drummond-Lage, A.P. Epidemiological and toxicological profile of homicide victims in a legal medicine unit in Brazil. J Forensic Leg Med 2019, 65, 55-60. [CrossRef]
- Sheehan, C.M.; Rogers, R.G.; Williams IV, G.W., Boardman, J.D. Gender differences in the presence of drugs in violent deaths. Addiction 2012, 108(3), 547-555.
- Weiner, M.D.; Sussman, S.; Sun, P.; Dent, C. Explaining the link between violence perpetration, victimization and drug use. Addict Behav 2005, 30(6), 1261-1266. [CrossRef]
- Dalgedan-Bueno, D.; Lindner, S.R.; Kovaleski, D.; Fischer, B. Cannabis use, risk behaviours and harms in Brazil: A comprehensive review of available data indicators. Drug Alcohol Rev 2023, 42(2), 318-336. [CrossRef]
- Stepjanovic, D.; Hall, W.; Leung, J. Illicit drug use and violence. In Handbook of Clinical Neurology, v 197 Brain and Crime; Swaab, H. Meynen, G., Ed.; Elsevier: Netherlands, 2023, 121-145.
- Boles, S.M.; Miotto, K. Substance abuse and violence: A review of the literature. Aggress Violent Behav 2003, 8(2), 155-174. [CrossRef]
- Dalgedan-Bueno, D.; Fischer, B. The association between cocaine product use and violence outcomes in Brazil: A comprehensive, systematized review. Aggress Violent Behav 2024, 101891. [CrossRef]
- Degenhardt, L.; Day, C.; Hall, W.; Conroy, E.; Gilmour, S. Was an increase in cocaine use among injectiong drug users in New South Wales, Australia, accompanied by an increase in violent crime? BMC Public Health 2005, 19:5:40. [CrossRef]
- Garrison, H.; Scholey, A.; Ogden, E.; Benson, S. The effects of alcohol intoxication on cognitive functions critical for driving: A systematic review. Accid Anal Prev 2021, 154:106052. [CrossRef]
- Borges, G.; Monteiro, M.; Cherpitel, C.J.; Orozco, R.; Ye, Y.; Poznyak, V.; Peden, M.; Pechansky, F.; Cremonte, M.; Reid, S.D.; Mendez, J. Alcohol and Road Traffic Injuries in Latin America and the Caribbean: A Case-Crossover Study. Alcohol Clin Exp Res 2017, 41(10), 1731-1737. [CrossRef]
- Bombana, H.S.; Bogstrand, S.T.; Gjerde, H.; Jamt, R.E.G.; Carvalho, H.B.; Andreuccetti, G.; Bernini, C.O.; Muñoz, D.R.; Leyton, V.; Greve, J.M.D. Use of alcohol and illicit drugs by trauma patients in Sao Paulo, Brazil. Injury 2022, 53(1), 30-36. [CrossRef]
- Pelição, F.S.; Peres, M.D.; Pissinate, J.F.; de Paula, D.M.L.; de Faria, M.G.C.; Nakamura-Palacios, E.M.; de Martinis, B.S. Predominance of alcohol and illicit drugs among traffic acidentes fatalities in an urban area of Brazil. Traffic Inj Prev 2016, 17(7), 663-667.
- Ponce, J.C.; Muñoz, D.R.; Andreuccetti, G.; de Carvalho, D.G.; Leyton, V. Alcohol-related traffic accidents with fatal outcomes in the city of Sao Paulo. Accident Anal Prev 2011, 43(3), 782-787. [CrossRef]
- Ponce, J.C.; Kawauti, M.C.P.; Andreuccetti, G.; Carvalho, H.B. Loaded dice: a game theory analysis of drunk driving laws in Brazil. Traffic Inj Prev 2018, 19(8), 794-798. [CrossRef]
- Centro de Excelência para a Redução da Oferta de Drogas Ilícitas – CdE. Tráfico de drogas na Amazônia. Achados iniciais. Available online: https://cdesc.org.br/publicacoes/. (accessed on 25/11/2025).
- Reuter, P. Systemic violence in drug markets. Crime Law Soc Change 2009, 52, 275-284. [CrossRef]
- Miron, J.; Partin, E. Ending the War on Drugs is an Essential Step Toward Racial Justice. Am J Bioeth 2021, 21(4), 1-3. [CrossRef]
- The Lancet. Editorial. Rethinking America’s “War on Drug” as a public-health issue. The Lancet 2001, 31, 357(9261),971.
| City | State | Brazilian geographical region | HDI* | External causes mortality rate/100,000* |
|---|---|---|---|---|
| Belém | Pará (PA) | North | 0.746 | 43.5 |
| Recife | Pernambuco (PE) | Northeast | 0.772 | 143.8 |
| Vitória | Espirito Santo (ES) | Southeast | 0.845 | 197.0 |
| Curitiba | Paraná (PR) | South | 0.885 | 80.4 |
| Analyte | Cutoff (ng/mL) | |
|---|---|---|
| Alcohol (g/L) | 0.2 | |
| Cannabis | ||
| ∆9-tetrahydrocannabinol (THC) | 1 | |
| Cocaine and metabolites | ||
| Cocaine | 20 | |
| Benzoylecgonine | 40 | |
| Cocaethylene | 20 | |
| Anhydroecgonine methyl ester (AEME – crack cocaine) | 20 | |
| Amphetamines | ||
| Amphetamine | 20 | |
| Methamphetamine | 20 | |
| MDMA (3,4-methylenedioxymethamphetamine - ecstasy) MDA (3,4-methylenedioxyamphetamine) |
20 | |
| 20 | ||
| Benzodiazepines | ||
| Clonazepam | 5 | |
| 7-aminoclonazepam | 5 | |
| Alprazolam | 5 | |
| Diazepam | 10 | |
| Bromazepam | 20 | |
| Oxazepam | 10 | |
| All deaths | Traffic-related | Homicides | Suicides | Poisoning | All others | |||||||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |
| n | 3,577 | 524 | 2,406 | 330 | 52 | 265 | ||||||
| General positivity | ||||||||||||
| At least one | 53.0 | (51.3-54.6) | 46.0 | (41.8-50.2) | 55.7 | (53.7-57.7) | 54.6 | (49.1-60.0) | 65.4 | (51.3-77.2) | 37.7 | (32.1-43.7) |
| Only alcohol | 16.6 | (15.4-17.9) | 30.9 | (27.1-35.0) | 14.5 | (13.2-16.0) | 14.5 | (11.1-18.8) | 5.8 | (1.8-16.8) | 12.5 | (8.9-17.0) |
| Only drugs | 21.6 | (20.3-23.0) | 5.5 | (3.9-7.9) | 27.3 | (25.5-29.1) | 10.9 | (7.9-14.8) | 32.7 | (21.2-46.8) | 12.8 | (9.3-17.5) |
| Two or more | 10.9 | (9.9-12.0) | 7.1 | (5.2-9.6) | 11.7 | (10.5-13.1) | 14.8 | (11.4-19.1) | 13.5 | (6.4-26.0) | 6.0 | (3.7-9.6) |
| Specific positivity | ||||||||||||
| Alcohol | 27.7 | (26.2-29.2) | 38.0 | (33.9-42.2) | 26.4 | (24.7-28.2) | 29.4 | (24.7-34.6) | 19.2 | (10.5-32.5) | 18.5 | (14.2-23.7) |
| Cocaine | 29.6 | (28.1-31.1) | 9.9 | (7.6-12.8) | 36.0 | (34.1-38.0) | 21.2 | (17.1-26.0) | 44.2 | (31.2-58.1) | 17.7 | (13.6-22.8) |
| Cannabis | 2.2 | (1.2-2.7) | 0 | 3.2 | (2.5-4.0) | - | - | 0 | - | - | ||
| Benzodiazepines | 6.8 | (6.0-7.7) | 4.4 | (2.9-6.5) | 4.8 | (4.0-5.8) | 20.3 | (16.3-25.0) | 25.0 | (14.9-38.8) | 9.0 | (6.1-13.2) |
| Alcohol + Cocaine | 9.8 | (8.8-10.7) | 5.2 | (3.6-7.4) | 10.9 | (9.7-12.2) | 11.5 | (8.5-15.4) | 13.5 | (6.4-26.0) | 5.3 | (3.1-8.7) |
| Alcohol + Cannabis | - | - | 0 | - | - | 0 | 0 | 0 | ||||
| Alcohol + Benzodiazepines | 1.7 | (1.4-2.2) | 1.9 | (1.0-3.5) | 1.3 | (1.0-1.9) | 4.2 | (2.5-7.0) | 3.9 | (1.0-14.5) | 1.5 | (1.0-4.0) |
| All victims | At least one | Any alcohol | Only alcohol | Only drugs | Two or more | |||||||
| % | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Sex | ||||||||||||
| Women | 10.9 | (9.9-11.9) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Men | 89.1 | (88.1-90.1) | 1.52 | (1.24-1.89)* | 1.06 | (0.85-1.31) | 1.16 | (0.87-1.57) | 1.92 | (1.42-2.61)* | 1.52 | (1.04-2.25)* |
| Age | ||||||||||||
| Less than 30 | 44.0 | (42.3-45.7) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| More than 30 or equal | 56.0 | (54.3-57.8) | 1.09 | (0.95-1.26) | 1.42 | (1.23-1.63)* | 1.94 | (1.59-2.36)* | 0.53 | (0.45-0.63)* | 1.11 | (0.89-1.39) |
| Race | ||||||||||||
| Non-white | 80.8 | (79.4-82.0) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| White | 19.2 | (18.0-20.6) | 1.17 | (0.98-1.40) | 2.52 | (2.12-3.03)* | 0.92 | (0.72-1.16) | 0.82 | (0.65-1.03) | 1.64 | (1.27-2.12)* |
| Injury type | ||||||||||||
| All others | 7.4 | (6.6-8.3) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Homicides | 67.3 | (65.7-68.8) | 2.00 | (1.51-2.66)* | 1.42 | (1.06-1.91)* | 1.38 | (0.93-2.08) | 1.98 | (1.32-2.95)* | 2.18 | (1.24-3.83)* |
| Traffic-related | 14.7 | (13.5-15.9) | 1.31 | (0.96-1.80) | 2.30 | (1.66-3.19)* | 3.27 | (2.13-5.02)* | 0.32 | (0.19-0.56)* | 1.22 | (0.64-2.32) |
| Suicide | 9.2 | (8.3-10.2) | 1.81 | (1.28-2.56)* | 2.12 | (1.49-3.02)* | 1.08 | (0.65-1.78) | 0.76 | (0.45-1.28) | 2.70 | (1.43-5.06)* |
| Poisoning | 1.4 | (1.1-1.9) | 2.78 | (1.40-5.51)* | 1.04 | (0.52-2.09) | 1.14 | (1.07-1.22) | 3.71 | (1.77-7.75)* | 2.62 | (0.94-7.27) |
| Death time | ||||||||||||
| Day | 46.1 | (44.3-47.9) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Night | 53.9 | (52.1-55.7) | 1.75 | (1.50-2.04)* | 1.36 | (1.17-1.59) | 2.00 | (1.61-2.48)* | 1.12 | (0.93-1.35) | 1.64 | (1.28-2.10)* |
| Death day | ||||||||||||
| Weekday | 62.6 | (61.0-64.2) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||
| Weekend | 37.4 | (35.8-39.0) | 1.52 | (1.32-1.76) | 1.52 | (1.31-1.76)* | 2.28 | (1.89-2.76)* | 0.84 | (0.70-1.01) | 1.41 | (1.13-1.78)* |
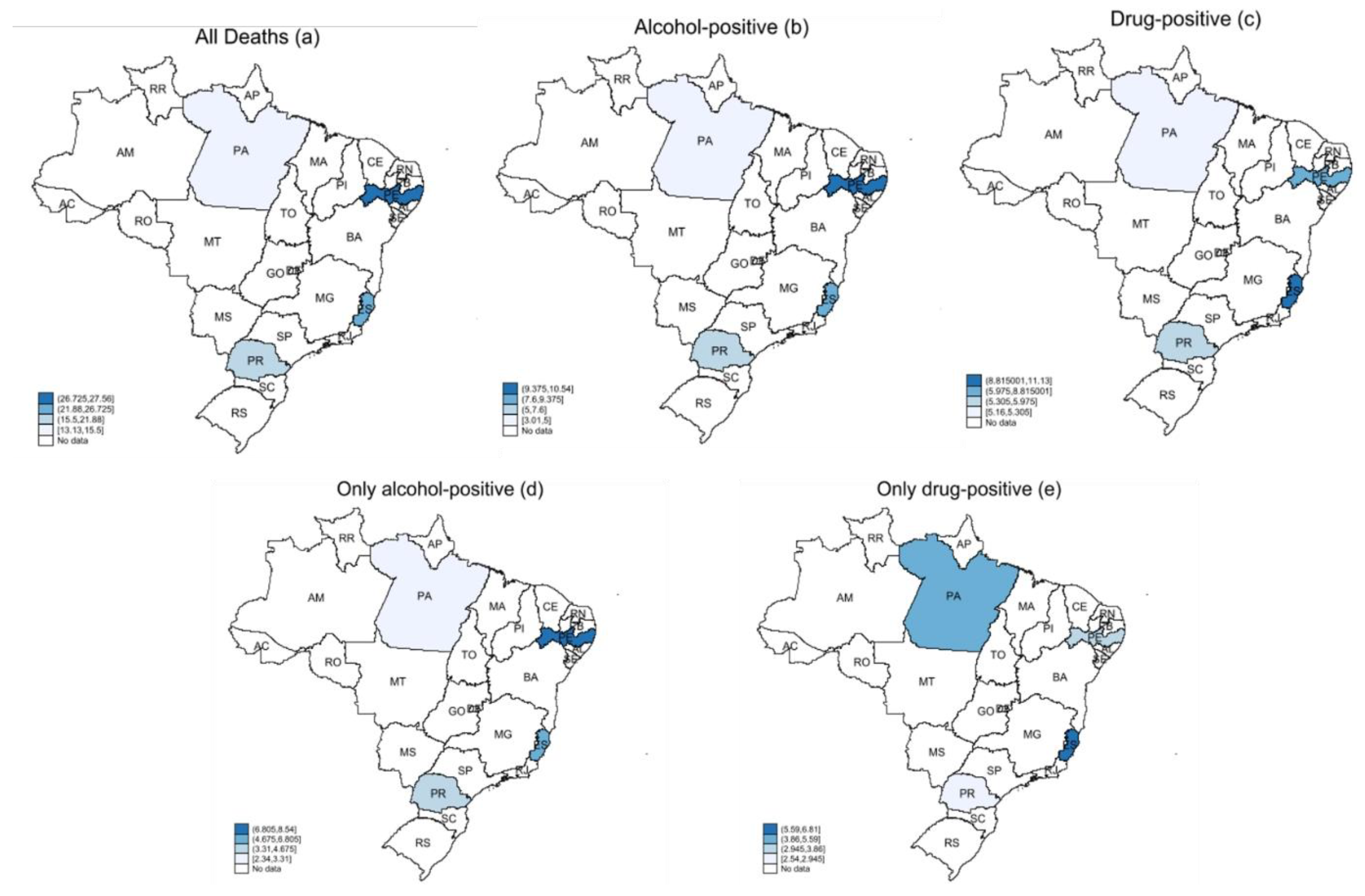
| Regions | All deaths | Alcohol-positive | Drug-positive | Only alcohol | Only drugs | DPR I | DPR II | |||||
| Mean | (95% CI) | Mean | (95% CI) | Mean | (95% CI) | Mean | (95% CI) | Mean | (95% CI) | |||
| PA - North | 13.13 | (5.48-20.78) | 3.01 | (1.55-4.48) | 5.16 | (1.12-9.20) | 2.34 | (1.03-3.66) | 4.37 | (0.66-8.09) | 1.57 | 1.95 |
| PE - Northeast | 27.56 | (21.90-33.23) | 10.54 | (7.92-13.15) | 6.50 | (4.62-8.38) | 8.54 | (6.41-10.67) | 3.35 | (2.26-4.44) | 0.80 | 0.57 |
| ES - Southeast | 25.89 | (21.77-30.01) | 8.21 | (6.21-10.21) | 11.13 | (8.05-14.20) | 5.07 | (2.51-7.63) | 6.81 | (3.47-10.16) | 1.39 | 1.39 |
| PR - South | 17.87 | (13.85-21.88) | 6.99 | (4.69-9.29) | 5.45 | (3.50-7.41) | 4.28 | (2.07-6.49) | 2.54 | (1.60-3.49) | 1.05 | 1.09 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





