1. Introduction
In recent decades, the healthcare sector has witnessed the growing adoption of new technologies, which has significantly influenced both the organization of services and the overall costs of care delivery. This trend has highlighted the need for evaluation tools that go beyond the assessment of clinical effectiveness alone, incorporating also economic and organizational dimensions.
Within this framework, Health Technology Assessment (HTA) has emerged as a multidimensional approach that integrates various methodologies. Among these, health economics analysis—such as cost-effectiveness analysis—plays a pivotal role, as it enables the estimation and comparison of costs while also considering clinical and social outcomes. When combined with technical, organizational, and managerial evaluations, HTA provides a comprehensive and systematic understanding of the impact of healthcare technologies.
One area where this approach is particularly relevant is robotic surgery, which has seen a marked increase in adoption over recent years and now represents one of the most significant innovations in modern surgical practice.
Over the past two decades, robotic-assisted surgery has evolved from a niche innovation into a widely adopted technology across multiple surgical specialties worldwide [
1,
2]. This rapid growth has been fueled by continuous technological progress, refined training protocols, and an expanding body of evidence supporting its clinical value. A pivotal milestone in this trajectory was the introduction of the Da Vinci Surgical System by Intuitive Surgical in 2000, one of the first robotic platforms to achieve widespread clinical implementation [
3].
By combining early market entry with a strategically constructed and comprehensive patent portfolio, the Da Vinci system secured a dominant position in the global market for nearly twenty years [
4,
5]. These patents, which covered both mechanical and software innovations, effectively prevented the emergence of meaningful competitors and established a near-monopoly. While this dominance accelerated innovation and adoption in certain contexts, it also enabled Intuitive Surgical to impose high acquisition, maintenance, and consumable costs. As a result, access to robotic surgery remained limited for many healthcare providers—particularly in low- and middle-income countries—exacerbating inequities in surgical care.
Despite these barriers, robotic-assisted surgery has consistently demonstrated substantial clinical and ergonomic benefits, including improved precision, reduced blood loss, shorter hospital stays, and enhanced working conditions for surgeons [
6,
7]. These advantages, widely recognized by the surgical community, have sustained global interest and demand for the technology. Anticipating the expiration of Intuitive Surgical’s key patents, several medical technology companies began investing in alternative robotic platforms to meet this demand.
In recent years, the end of these patent protections has opened the field to new competitors [
8,
9]. Among the most prominent entrants are the Hugo™ Robotic-Assisted Surgery (RAS) System, developed by Medtronic, and the Versius
® Surgical Robotic System, introduced by CMR Surgical. These systems aim not only to match the clinical performance of Da Vinci but also to provide more cost-effective, modular, and workflow-friendly solutions. Their introduction has ushered in a new phase of competition, fostering innovation, increasing market dynamism, and potentially lowering the overall costs of robotic surgery, thereby improving accessibility on a global scale [
4,
8,
9].
The Clinical Engineering Department of ASST Grande Ospedale Metropolitano Niguarda Hospital conducted a cost-minimization analysis and a break-even analysis to assess which of the three robotic platforms currently in use at the institution could generate the greatest economic savings and return on investment as surgical volumes increase. While some studies have reported economic evaluations of robotic surgery at the per-procedure level, to the best of the authors’ knowledge, no previous analyses have directly compared the three platforms using both cost-minimization and break-even methodologies.
For this purpose, radical prostatectomy was selected as the reference procedure, given that it is the intervention with the most comprehensive data available in the literature and, within the hospital itself, the procedure with the highest surgical volume. This choice ensures a robust basis for comparison across the platforms.
Economic analyses of this kind are of particular relevance within a hospital setting, as they provide decision-makers with a structured framework for comparing technologies and optimizing resource allocation.
2. Materials and Methods
2.1. Study Design
A comparative economic evaluation was conducted by the Clinical Engineering Department of ASST Grande Ospedale Metropolitano Niguarda Hospital to assess the economic sustainability of three robotic surgical platforms currently in use at the institution. The analysis included a cost-minimization analysis (CMA) and a break-even analysis (BEA).
2.2. Literature Search
A literature search of the economic aspects was conducted to support the comparative analysis of the three robotic platforms currently in use at ASST Grande Ospedale Metropolitano Niguarda Hospital. The objective of this search was to identify studies reporting economic evaluations of robotic-assisted surgery, with specific attention to cost analyses relevant to radical prostatectomy. Particular emphasis was placed on methodologies, type of economic evaluation, results, and applicability within the Italian healthcare context.
It has been searched in PubMed, Scopus and Web of Science. Grey literature, including HTA reports, was retrieved from the websites of major HTA agencies.
The research strategy was (“Hugo” OR “Versius”) AND “Da Vinci” AND “cost”
The following are the Inclusion criteria:
Systematic reviews, clinical trials, prospective or retrospective studies, and HTA reports published in English;
Studies published between 2019 and 2025;
Articles reporting cost analyses of robotic-assisted surgery compared to conventional alternatives;
Following the Exclusion criteria are reported:
Case reports, editorials, letters, or conference abstracts without full text;
Studies focusing exclusively on clinical outcomes without economic evaluation;
Simulation-only or non-human studies.
All retrieved titles and abstracts were screened for relevance, followed by full-text review of potentially eligible studies.
The final evidence set was used to validate assumptions on clinical comparability across robotic platforms, to benchmark cost components, and to highlight the gap in the literature regarding cost-minimization and break-even analyses comparing multiple robotic systems.
2.3. Procedure Selection
Radical prostatectomy was selected as the reference procedure due to its high surgical volume within the hospital and the extensive availability of outcome and cost data in the literature.
2.4. Data Collection
Both fixed and variable costs were determined by integrating evidence from the literature with information provided by the robotic system manufacturer and data extracted from the hospital management system. Additional cost input was derived from the hospital’s administrative and financial records, covering expenses such as system acquisition, annual maintenance contracts, consumables, and operating room utilization.
2.5. Cost Minimization Analysis and Break-Even Analysis
Break-even and cost-minimization analyses were conducted, drawing on evidence from the literature and data extracted from the hospital management system.
For the cost analysis, we started defining the cost drivers. These include costs of the robot, cost of consumable, costs of personnel, costs of the operatory room (electricity, anaesthesia, other medical devices), costs of hospital stay.
As current evidence suggests that the new robotic platforms provide clinical outcomes comparable to those of the Da Vinci system, a cost-minimization analysis was conducted. CMA is a special form of cost-effectiveness analysis in which the efficacy of all surgical alternatives is considered equal. Thus, it was focused solely on identifying the strategy with the lowest cost of the three.
Under this assumption of clinical equivalence, the analysis focused exclusively on identifying the platform associated with the lowest overall cost.
In parallel, a break-even analysis was developed to estimate the minimum number of surgical procedures required annually for each platform to achieve cost recovery. This approach identifies the point at which total revenues equal total costs. Beyond serving as a benchmark, the BEA also allowed exploration of multiple scenarios through sensitivity testing.
Both the break-even and cost-minimization analyses were performed using evidence from the literature, internal data extracted from the hospital management system, and the expertise of the Clinical Engineering Department.
3. Results
The comparative economic evaluation was performed using cost-minimization and break-even analyses to assess differences in cost efficiency among the three robotic surgical platforms: Da Vinci, Hugo™, and Versius®.
The following sections identify the platform with the lowest cost per procedure, and present the estimated break-even points based on surgical volume.
3.1. Literature Search Results
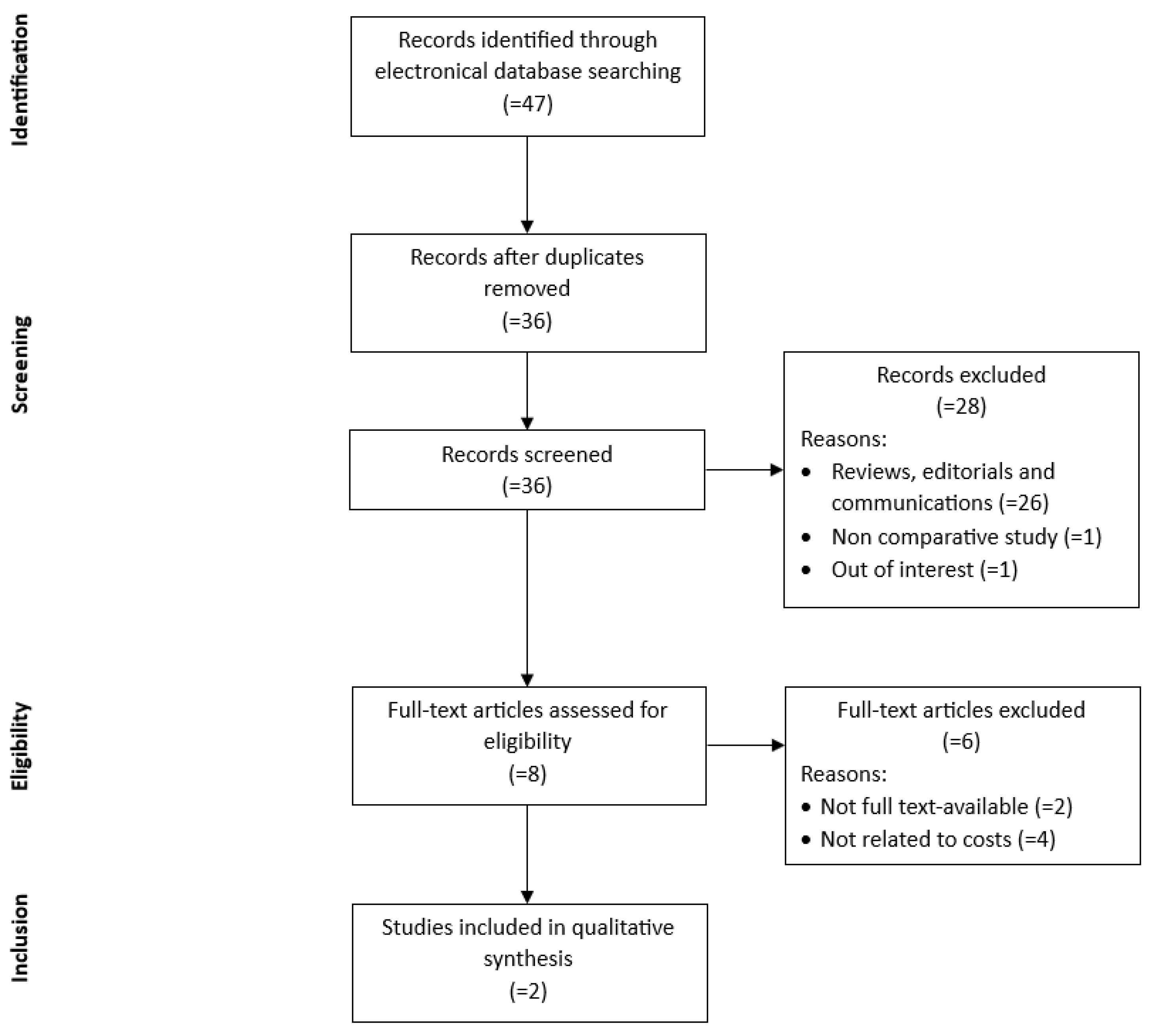
A total of 47 articles was obtained from the electronic research databases previously mentioned. After duplicates were removed, 36 papers remained. The screening of the titles and abstracts resulted in the exclusion of 28 items. Among the remaining 8 articles, 6 papers did not meet the inclusion criteria. The selection process is reported in the PRISMA flowchart (
Figure 1).
A cost projection study [
10] from a public robotic surgery center in Milan compared Da Vinci and Hugo RAS systems for robot-assisted radical prostatectomy. Among 41 cases (27 Da Vinci, 14 Hugo RAS), perioperative outcomes were comparable, though operative time was longer with Hugo RAS. The per-procedure cost was lower for Hugo RAS (€1,995 vs €2,246), yielding an estimated 11% saving in total hospitalization costs (€6,637 vs €6,775). The authors conclude that Hugo RAS provides similar clinical results with a modest cost advantage over the Da Vinci system.
Similarly, an analysis [
11] from the Azienda Ospedaliera Universitaria Integrata Verona (Italy) compared the costs of robot-assisted radical prostatectomy performed with the Da Vinci and Hugo RAS platforms using a Time-Driven Activity-Based Costing approach. Among 100 patients (50 per platform), clinical outcomes were comparable, but Hugo RARP was less expensive overall (€3,512 vs €4,979; p < 0.001). While intraoperative time and personnel costs were higher with Hugo, this was offset by substantially lower material and kit costs. Sensitivity analyses confirmed that surgical kit price was the most influential factor in cost differentials, indicating that Hugo RAS offers a cost advantage under comparable clinical performance.
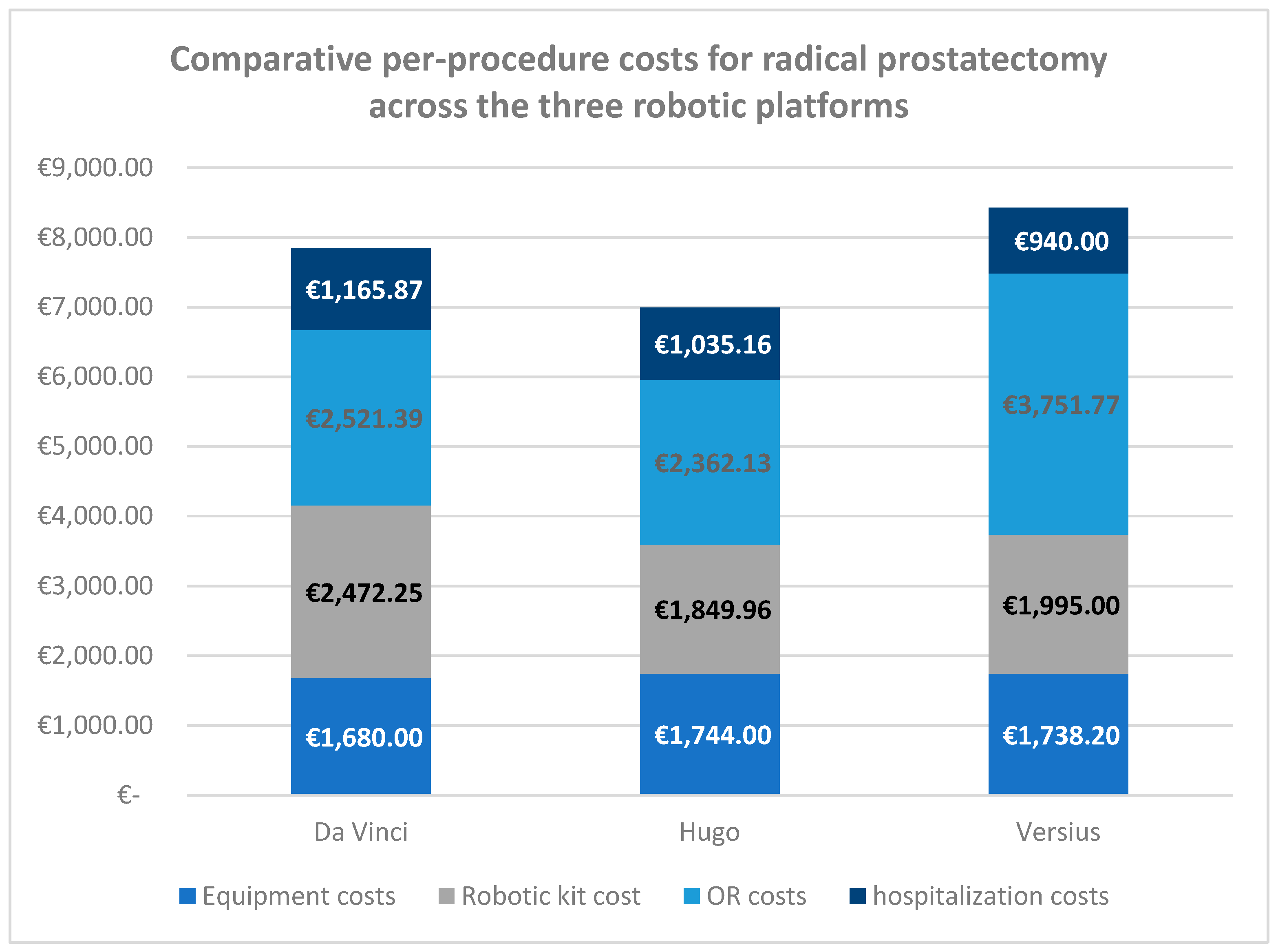
3.2. Cost Minimization Analysis
The cost-minimization analysis was performed under the assumption of clinical equivalence among the three robotic platforms, as supported by the available literature. The analysis focused on identifying the system associated with the lowest overall cost per radical prostatectomy, considering both fixed and variable cost components.
Fixed costs included system acquisition and annual maintenance, while variable costs comprised consumables, operating room time, and personnel expenses. All costs were standardized and expressed in euros (€), based on data from literature and data from ASST Grande Ospedale Metropolitano Niguarda Hospital.
The CMA compared the per-procedure costs of radical prostatectomy performed with the three robotic platforms currently in use at ASST Grande Ospedale Metropolitano Niguarda Hospital: Da Vinci, Hugo™, and Versius
®. The results are summarized in
Table 1.
Under the assumption of clinical equivalence, the Hugo™ system demonstrated the lowest overall cost per procedure, amounting to €6,991.26, followed by the Da Vinci system at €7,839.51, and the Versius® system at €8,424.97.
When analyzing individual cost components, the Hugo™ platform presented the lowest kit cost (€1,849.96) and operating room cost (€2,362.13), while Versius® achieved the lowest hospitalization cost (€940.00). Equipment costs were comparable across all systems, ranging from €1,680.00 (Da Vinci) to €1,744.00 (Hugo™).
The largest cost differentials were observed in operating room and kit-related expenses, which together represented the main drivers of total cost variation among the platforms. Specifically, Hugo™ showed a cost advantage of approximately €848 per procedure compared to Da Vinci and €1,434 per procedure compared to Versius®.
Overall, the CMA findings indicate that, within the current hospital context and assuming comparable clinical outcomes, the Hugo™ robotic platform represents the most cost-efficient option for radical prostatectomy. These results highlight the potential for substantial cost savings primarily through reduced consumable and operating room expenditures.
Figure 2 illustrates the comparative distribution of costs per radical prostatectomy across the three robotic platforms analyzed — Da Vinci, Hugo™, and Versius
®. The figure provides a visual representation of the contribution of each cost component (equipment, kit, operating room, and hospitalization) to the total per-procedure cost.
As shown in the graph, the Hugo™ system consistently demonstrates lower expenditures in most categories, particularly for kit and operating room costs, which together account for the majority of the overall savings. The Da Vinci system shows intermediate values across all components, whereas the Versius® platform presents the highest total cost, mainly driven by longer operating room time and higher associated expenses.
The visual comparison clearly highlights that cost differentials among platforms are primarily driven by variable cost components, while fixed equipment costs remain relatively uniform. This pattern reinforces the findings of the CMA, indicating that optimization of consumable utilization and operating room efficiency are the key levers for achieving cost reduction in robotic-assisted radical prostatectomy.
3.3. Break-Even Analysis
To complement the cost-minimization analysis, a break-even analysis was conducted to estimate the minimum annual number of radical prostatectomy procedures required for each robotic platform to recover total costs. The BEA considers both fixed costs (equipment acquisition and annual maintenance) and variable costs per procedure (kit, operating room, hospitalization), allowing a comprehensive assessment of economic sustainability under different utilization scenarios.
Procedure revenues were based on the Diagnosis-Related Group (DRG) tariffs established by Lombardy Region, ensuring that the break-even estimates reflect actual reimbursement rates applicable to the hospital and providing a realistic assessment of economic sustainability. The Lombardy Region’s DRG robot-assisted radical prostatectomy amount to €8,777 per procedure.
The BEA results indicate substantial differences in the minimum annual case volume required for cost recovery across the three platforms (
Figure 2). The Hugo™ system reaches break-even at approximately 124 procedures per year, reflecting its lower total per-procedure cost. The Da Vinci system achieves break-even at around 161 procedures per year, whereas Versius
® requires approximately 208 procedures per year, primarily due to higher overall costs. In
Figure 3 the break-even points across the three platforms are shown, they represents the minimum number of annual procedures required to recover total costs, based on fixed and variable cost components and DRG reimbursement of €8,777 per procedure from Lombardy Region.
These findings highlight that the number of procedures necessary to achieve cost recovery is strongly influenced by per-procedure variable costs, particularly kit and operating room expenses, while fixed equipment costs remain relatively uniform across platforms.
4. Discussion
This study provides a comparative economic assessment of three robotic surgical platforms—Da Vinci, Hugo™, and Versius®—currently in use at ASST Grande Ospedale Metropolitano Niguarda Hospital, with the objective of identifying the most cost-efficient solution for radical prostatectomy. By combining hospital-level data with evidence from the literature, the analysis offers a detailed overview of the economic sustainability of each system, focusing on both per-procedure costs and the volume thresholds required to achieve financial equilibrium.
The cost-minimization analysis revealed that the Hugo™ platform achieved the lowest total per-procedure cost (€6,991.26), followed by Da Vinci (€7,839.51) and Versius® (€8,424.97). The main cost differentials were driven by consumable and operating room expenditures, whereas equipment and hospitalization costs remained relatively uniform across platforms. These findings suggest that opportunities for cost reduction in robotic-assisted surgery are more likely to arise from optimizing variable resources—such as kit utilization and operating room efficiency—rather than from reductions in capital expenditure.
The break-even analysis further supported these results, showing that the Hugo™ platform reached cost recovery at approximately 124 procedures per year, compared with 160 procedures for Da Vinci and 208 for Versius®. Considering the DRG tariff for robot-assisted radical prostatectomy established by Regione Lombardia (€8,777 per procedure), the analysis indicates that the economic sustainability of robotic systems depends heavily on procedural volume. Hospitals with higher surgical throughput are more likely to achieve financial balance, whereas centers with lower case volumes may face challenges in recovering investment costs, particularly when using platforms with higher per-procedure expenses.
From a managerial and strategic perspective, these findings emphasize the importance of aligning case volume, resource allocation, and reimbursement levels when introducing or expanding robotic surgery programs. In addition, the emergence of new competitors such as Hugo™ and Versius® marks an important step toward the democratization of robotic surgery, potentially fostering price competition and greater accessibility within public healthcare systems.
Nevertheless, several limitations should be acknowledged. The analysis was limited to the urology field and focused exclusively on radical prostatectomy; therefore, the results cannot be directly generalized to other surgical specialties. Furthermore, the study relied on a relatively small dataset, combining hospital records and literature-derived information, which introduces a degree of uncertainty and variability in the estimates. As a consequence, cost differentials across platforms should be interpreted with caution. Additionally, the analysis adopted a hospital-based perspective and did not account for indirect costs such as training, learning curve effects, or long-term maintenance variations.
In conclusion, within the evaluated context and under the assumption of clinical equivalence, the Hugo™ system emerged as the most cost-efficient and economically sustainable option for robot-assisted radical prostatectomy. However, the observed variability in cost performance underscores the need for institution-specific evaluations and volume-based planning when selecting robotic technologies. Future research should extend this analysis to other surgical fields and larger datasets to confirm these findings and to support evidence-based decision-making in the ongoing evolution of robotic surgery.
Author Contributions
Conceptualization, P.P. and V.C.; methodology, P.P., C.L, G.P., F.S., I.G., U.N and V.C.; formal analysis, V.C.; writing—original draft preparation, P.P. and V.C.; writing—review and editing, P.P., C.L, G.P., F.S., I.G., U.N, and V.C.; supervision, P.P., C.L, G.P., F.S., I.G., U.N, and V.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data supporting the conclusions of this article are available from ASST Grande Ospedale Metropolitano Niguarda, but they are subject to restrictions, as they were accessed under license for the purposes of this research and so are not publicly available. The data are, however, available from the authors upon reasonable request and with the permission of ASST Grande Ospedale Metropolitano Niguarda.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HTA |
Health Technology Assessment |
| RAS |
Robotic-Assisted Surgery |
| CMA |
Cost-Minimization Analysis |
| BEA |
Break-Even Analysis |
| DRG |
Diagnosis-Related Group |
References
- A. L. G. Morrell et al., “The history of robotic surgery and its evolution: When illusion becomes reality,” Rev Col Bras Cir, vol. 48, pp. 1–9, 2021. [CrossRef]
- L. Maynou, G. Pearson, A. McGuire, and V. Serra-Sastre, “The diffusion of robotic surgery: Examining technology use in the English NHS,” Health Policy (New York), vol. 126, no. 4, pp. 325–336, Apr. 2022. [CrossRef]
- F. Pugin, P. Bucher, and P. Morel, “History of robotic surgery: From AESOP¯ and ZEUS¯ to da Vinci¯,” J Visc Surg, vol. 148, no. 5, pp. e3–e8, Oct. 2011. [CrossRef]
- N. Mayor, A. S. Coppola, and B. Challacombe, “Past, present and future of surgical robotics,” Trends in Urology & Men’s Health, vol. 13, no. 1, pp. 7–10, Jan. 2022. [CrossRef]
- R. Liu, Q. Liu, and Z. Wang, “Worldwide diffusion of robotic approach in general surgery,” Jun. 01, 2021, Springer Science and Business Media Deutschland GmbH. [CrossRef]
- H. Ashrafian, O. Clancy, V. Grover, and A. Darzi, “The evolution of robotic surgery: Surgical and anaesthetic aspects,” in British Journal of Anaesthesia, Oxford University Press, Dec. 2017, pp. i72–i84. [CrossRef]
- S. Kutana, D. P. Bitner, P. Addison, P. J. Chung, M. A. Talamini, and F. Filicori, “Objective assessment of robotic surgical skills: review of literature and future directions,” Jun. 01, 2022, Springer. [CrossRef]
- P. Picozzi et al., “Advances in Robotic Surgery: A Review of New Surgical Platforms,” Dec. 01, 2024, Multidisciplinary Digital Publishing Institute (MDPI). [CrossRef]
- F. Marchegiani et al., “New Robotic Platforms in General Surgery: What’s the Current Clinical Scenario?,” Jul. 01, 2023, Multidisciplinary Digital Publishing Institute (MDPI). [CrossRef]
- M. C. Sighinolfi et al., “Cost analysis of new robotic competitors: a comparison of direct costs for initial hospital stay between Da Vinci and Hugo RAS for radical prostatectomy,” J Robot Surg, vol. 18, no. 1, pp. 1–4, Dec. 2024. [CrossRef]
- S. Landi, G. Maistri, L. P. Orsini, C. Leardini, S. Malandra, and A. Antonelli, “Supporting managerial decisions: a comparison of new robotic platforms through time-driven activity-based costing within a value-based healthcare framework,” BMC Health Serv Res, vol. 25, no. 1, pp. 1–12, Dec. 2025. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).