1. Introduction
Bone fractures represent a significant challenge for health systems, given the anatomical complexity of the craniofacial region and the serious consequences that these injuries can have on the patient's functionality and aesthetics. These traumas, often caused by traffic accidents, interpersonal violence, falls and sporting activities, compromise specific functions such as breathing, vision and chewing, as well as impacting the quality of life and psychological well-being of affected individuals. Adequate care for these cases requires specialized hospital resources, making it a relevant public health problem [
1,
2,
3,
4].
In the state of Paraíba, the Unified Health System (SUS) is the main provider of treatment for physical fractures, especially for low-income populations who depend on the public system. The SUS uses Hospital Admission Authorizations (AIH) as a mechanism to finance and monitor this care, recording specific hospital procedures and enabling a detailed analysis of the demand for health services. An analysis of IHAs related to the treatment of bone fractures provides an understanding of the distribution of care in the state, identifying variations between different hospitals and regions and revealing temporal patterns that may reflect changes in exposure to risk factors [
6,
7].
Understanding the epidemiology of facial bone fractures in the state of Paraíba is important for developing health policies that meet local needs, especially in a context of regional inequalities and challenges in access to health care. The state, with a combination of urban and rural areas, presents different risk factors: in urban areas, traffic accidents and interpersonal violence are frequent causes of apparent fractures, while in rural areas, work-related accidents and limitations in safety infrastructure are also important for these traumas. In addition, care capacity and the availability of specialized resources can vary significantly between different hospital establishments [
7,
8,
9].
The aim of this study is to carry out an epidemiological analysis of IHAs approved for the treatment of body fractures in Paraíba hospitals between 2014 and 2024.Using a comparative approach between the state's main hospitals and a temporal analysis over the decade, we aim to identify regional and temporal patterns that can inform prevention policies and resource allocation.It is hoped that the results of this research will provide input for more effective and equitable health planning in Paraíba, improving care and simplifying disparities in access to treatment for facial trauma.
2. Materials and Methods
This is an observational and descriptive study, with a retrospective approach, using secondary data previously collected and recorded in the DATASUS system [
10]. This approach made it possible to assess the historical demand for bone fracture treatment in the state of Paraíba. The data used in this study was obtained from the DATASUS system, specifically the SUS Hospital Information System (SIH/SUS), which records Hospital Admission Authorizations (AIH) approved for various health procedures, including the treatment of bone fractures.
The period analyzed was from September 2014 to September 2024. The study population included all IHA records for procedures associated with the treatment of bone fractures carried out in hospitals in the state of Paraíba during the analysis period, allowing for a comprehensive and representative assessment of the demands for treatment of metal fractures in different regions of the state. The various types of procedures related to the treatment of bone fractures were considered for analysis, such as osteosynthesis of mandibular, zygomatic and maxillary fractures, as specified in the table extracted from the DATASUS system. These procedures were selected because they are directly related to facial trauma care, according to the codes recorded in the system.
The methodology involves compiling and tabulating data extracted from DATASUS, with the aim of identifying and analyzing temporal and regional patterns in the distribution of approved AIHs. Based on this data, a descriptive analysis was carried out to assess the distribution of approvals over the years and between the different hospital establishments. In order to facilitate the interpretation of the data and the identification of trends, descriptive statistical methods were applied, including counts and percentages. The results were organized in tables and graphs, providing a clear visualization of the temporal and regional variations in the approval of AIH for the treatment of bone fractures.
3. Results
The analysis of Hospital Admission Authorizations (AIH) approved for the treatment of bone fractures in Paraíba between 2014 and 2024 allows us to identify important patterns in terms of demand, complexity of procedures, hospital distribution and associated factors such as length of stay and deaths. This data is important for understanding the health system's capacity to deal with physical trauma, as well as for targeting improvements in hospital care and resource planning.
Distribution by type of procedur
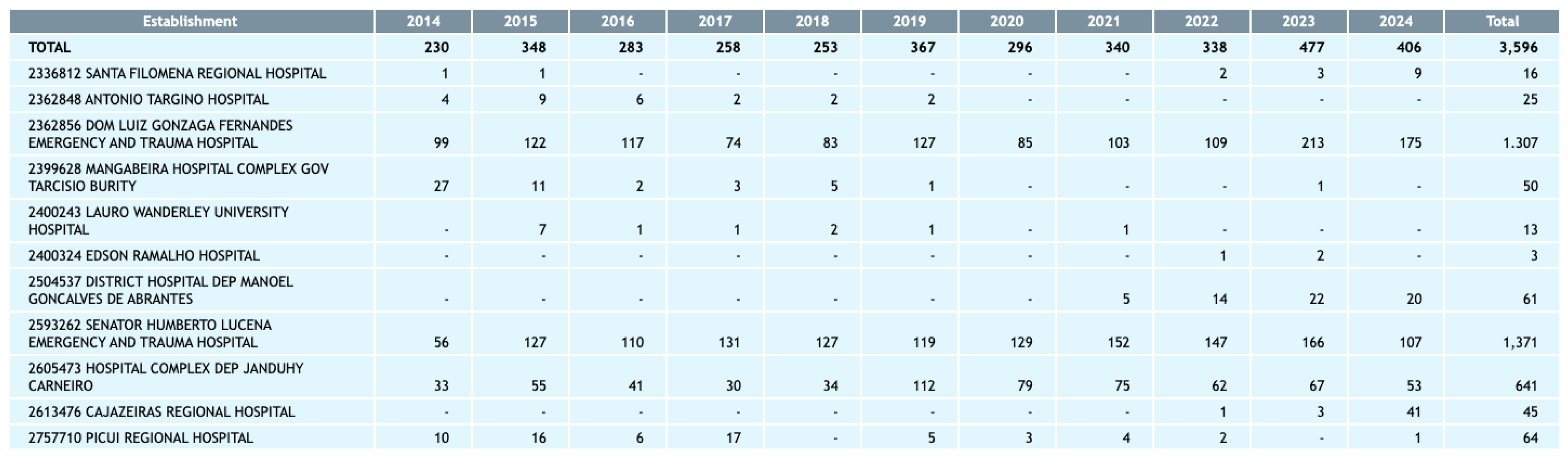
Over the specific period, a total of 3,595 IHAs were approved for different bone fracture treatment procedures (
Figure 1). The most frequent procedures included “Osteosynthesis of complex fracture of the mandible” (864 approvals) and “Osteosynthesis of fracture of the orbito-zygomatic-maxillary complex” (745 approvals), together accounting for more than 44% of all IHAs. These figures suggest that the majority of industrial fractures treated are highly complex, reflecting serious injuries that require extensive surgical interventions to stabilize multiple bony structures of the face. The predominance of these procedures points to a demand for technical expertise and developed infrastructure in hospitals that carry out such treatments, since these surgical procedures involve considerable risks and require a multidisciplinary team, including oral and maxillofacial surgeons, anesthesiologists and intensive care specialists.
Other procedures also had significant numbers, such as “Surgical treatment of zygomatic bone fracture without osteosynthesis” (616 approvals) and “Osteosynthesis of simple mandible fracture” (376 approvals). Less frequent procedures, such as “Reduction of alveolodental fracture without osteosynthesis” and “Osteosynthesis of bilateral mandibular condyle fracture”, accounted for 33 and 45 approvals respectively, showing a lower prevalence of alveolodental and mandibular condyle injuries among the patients seen. The variation in the types of procedures approved reflects the diversity of protected surgical fractures, ranging from simple, localized injuries to complex traumas involving several regions of the face.
Temporal analysis
The annual evolution of IHA approvals shows an upward trend, culminating in 2023 with the highest number of approved hospitalizations (481) (
Figure 2). Compared to 2014, which saw 232 AIHs, this is an increase of more than 100% over the course of a decade. This growth may be associated with several factors, including the increase in the urban population and the growth in risk factors such as traffic accidents and violence, which are common causes of apparent fractures. The increase may also indicate improvements in the process of diagnosing and reporting these traumas, as well as an expansion in the care capacity of referral hospitals. The slight reduction observed in 2024, with 410 AIH approved, suggests a possible stabilization in demand or a seasonal variation that may be related to changes in the rates of accidents and violent incidents. This temporal pattern highlights the importance of continuously monitoring risk factors for mechanical fractures, allowing health authorities to respond proactively to changes in demand for trauma services.
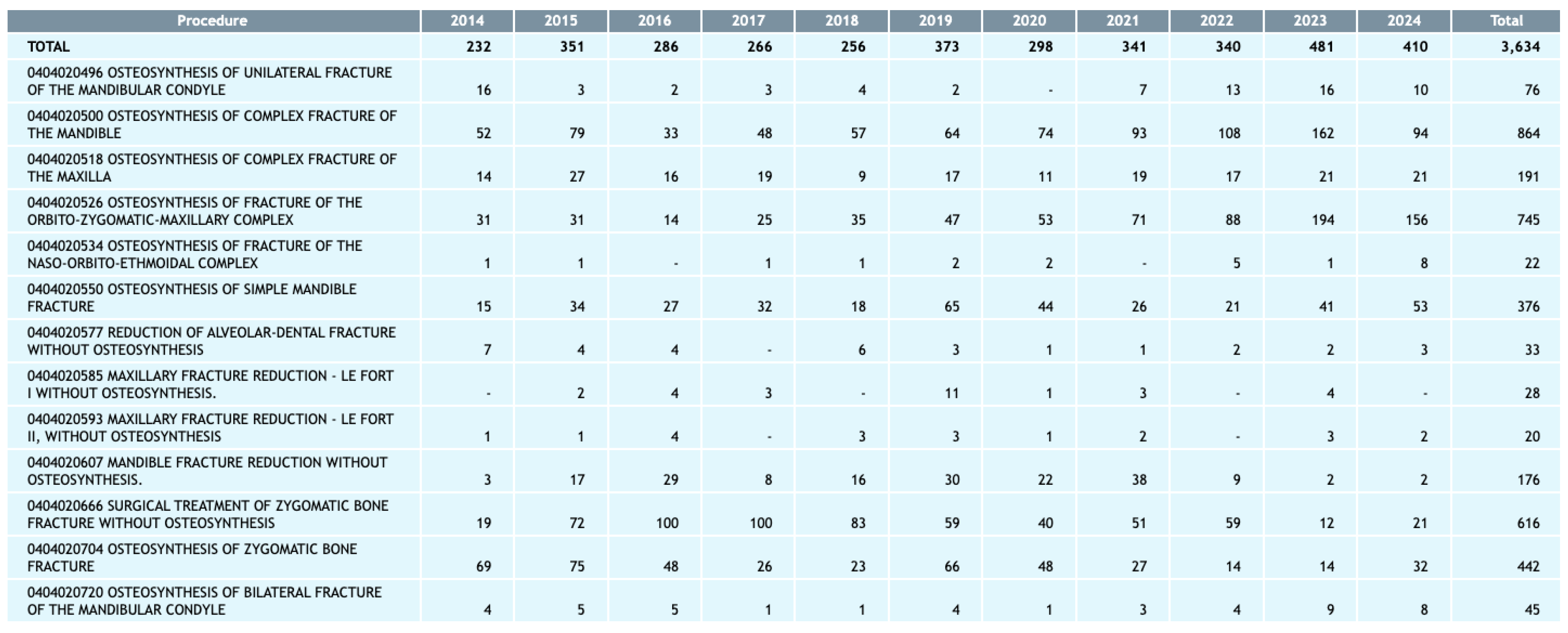
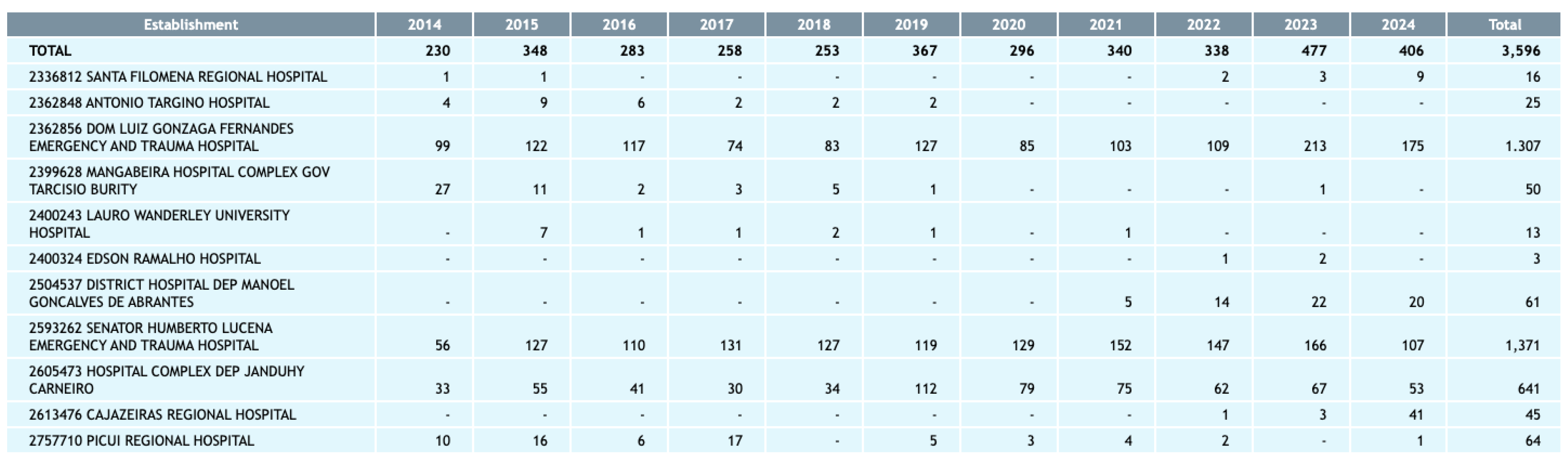
Distribution by hospital
The concentration of approvals in certain hospitals reveals the centralization of specific trauma care in Paraíba's main referral centers. The Dom Luiz Gonzaga Fernandes Emergency and Trauma Hospital and the Senador Humberto Lucena Emergency and Trauma Hospital were responsible for 1,371 and 1,307 approvals, respectively. These hospitals, located in urban regions with high population density, have the infrastructure and specialized teams to deal with complex cases, which justifies the high volume of admissions. The Complexo Hospitalar Deputado Janduhy Carneiro also had a significant number of approvals, with 641 AIH, indicating its importance in the specific trauma care network.
Smaller hospitals, such as the Cajazeiras Regional Hospital and the Lauro Wanderley University Hospital, recorded a lower annual average of AIH approvals, between 1.7 and 1.8, respectively, but play an important role for the population living in areas further away from the major centers. This unequal distribution between large and smaller hospitals suggests that the demand for more complex procedures is technically higher in hospitals with greater technical capacity and infrastructure. This reflects a strategy of regionalization of care, but it also raises questions about equitable access to facial trauma treatment for patients living far from major centers.
Deaths related to treatment
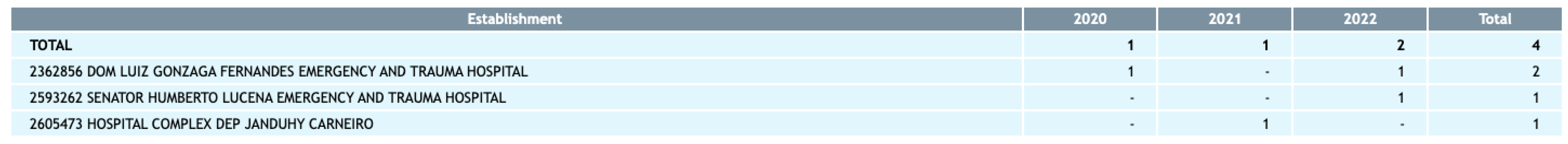
Mortality associated with the treatment of bone fractures was low (
Figure 3), with four deaths recorded over the period. Two of these deaths occurred at the Dom Luiz Gonzaga Fernandes Emergency and Trauma Hospital, while the Senador Humberto Lucena Emergency and Trauma Hospital and the Deputado Janduhy Carneiro Hospital Complex registered one death each. Although the number of deaths is low, it indicates that some cases of bone fractures are serious enough to result in fatal complications, possibly due to the complexity of the trauma, the presence of comorbidities or post-operative complications. These data suggest that, despite the low mortality rate, there is a need for specific care protocols to minimize risks and ensure safe and effective treatment, especially for critically ill patients.
Average hospital stay
The average hospital stay varies specifically between hospitals, with an overall average of 6.5 days (
Figure 4). The Dom Luiz Gonzaga Fernandes Emergency and Trauma Hospital had the longest average stay, at 8.5 days, while the Senador Humberto Lucena Emergency and Trauma Hospital recorded an average of 4.7 days. This difference can be explained by the complexity of the cases treated at each hospital. The longer average stay at Dom Luiz Gonzaga Fernandes Hospital may be associated with the care of more serious cases, which require a prolonged recovery period and intensive monitoring. On the other hand, the shorter length of stay at the Senador Humberto Lucena Hospital may indicate a higher turnover of beds and an approach to medium-complexity cases, with a shorter recovery time. The average hospital stay is an important indicator of the severity of the cases treated and the hospital's ability to manage the demand for beds, especially in highly complex trauma units.
The data shows a growing demand for bone fracture care in Paraíba, with a significant concentration of AIH approvals in large, specialized hospitals. The annual growth in AIH approvals and the concentration of complex procedures in reference hospitals highlight the need for continuous support in these centers, as well as investments in training and infrastructure. The distribution of procedures and the average length of hospital stay highlight the need for an integrated care network that can manage both highly complex cases and less serious injuries in regional hospitals.
Although the number of deaths is low, the analysis reinforces the importance of safety and prevention policies to reduce the incidence of severe trauma, as well as safe clinical practices to minimize complications and promote better outcomes. These findings provide a solid basis for public health planning, targeting investments in strategic hospitals and considering the need to decentralize care to ensure access to human trauma treatment in all regions of the state.
4. Discussion
The results of this study reveal a growing demand for facial fracture care in Paraíba, as well as a significant concentration of this care in large, specialized hospitals. These findings reflect both the complexity of facial trauma and the distribution of hospital resources and capacities in the state. The high frequency of complex procedures, such as osteosynthesis of mandibular fractures and fractures of the orbito-zygomatic-maxillary complex, indicates that the majority of cases treated involve serious injuries, which raises important questions about the allocation of resources and the infrastructure needed to manage these cases.
The temporal analysis shows a significant increase in hospital admission authorizations (AIH) over the years, with a peak in 2023. This growth can be attributed to various factors, such as population and urban growth, which is generally associated with a higher incidence of traffic accidents and interpersonal violence, two common causes of facial fractures [
11,
12].
The increase may also be related to a possible improvement in the notification and diagnosis of these cases, indicating that health systems are better prepared to identify and record facial trauma. These data suggest that, in order to sustainably meet the growing demand, Paraíba's health system may need to expand its specialized care capacity, mainly in large centers, but also in regional hospitals to ensure access in peripheral areas [
13,
14].
The concentration of AIH approvals in reference hospitals, such as the Dom Luiz Gonzaga Fernandes Emergency and Trauma Hospital and the Senador Humberto Lucena Emergency and Trauma Hospital, highlights the importance of these centers as pillars of facial trauma care in the state. This centralization of care is common in health systems that rely on high-capacity hospitals for complex treatments, but it also points to a possible weakness in the decentralization of care. Dependence on a few hospitals to carry out most complex procedures can overload these units and limit access for patients in distant regions. This scenario raises the need to consider expanding infrastructure and training in regional hospitals to distribute the care load and ensure that patients across the state have timely access to specialized care [
15,
16].
Another important point is the mortality rate associated with the treatment of facial fractures, which, although low, is notable for the seriousness that some of these cases can have. Although the number of deaths is small, it highlights the complexity of certain facial traumas and the need for strict safety protocols and well-trained teams to minimize risks during care and the post-operative period. Complications can occur due to the nature of the trauma, the presence of comorbidities or even the lack of adequate resources to manage critical cases. This suggests that, even with a limited number of deaths, care policies should include continuous training and investment in advanced support equipment to improve patient safety [
17,
18,
19].
The average length of stay varied between the hospitals, reflecting differences in the profile of the patients and the complexity of the cases treated. Dom Luiz Gonzaga Fernandes Hospital, with an average stay of 8.5 days, indicates a greater focus on highly complex cases that require a longer recovery and intensive follow-up. In contrast, the Senador Humberto Lucena Hospital, with an average of 4.7 days, may be dealing with medium-complexity cases or have a structure that allows for a more agile recovery. Length of stay is an important indicator of a hospital's efficiency and ability to cope with the demand for beds, especially in an environment where the volume of facial trauma is high. These data also suggest that hospitals with longer lengths of stay need more resources to manage complex cases, while hospitals with shorter lengths of stay can benefit from strategies to increase turnover and free up beds for new patients [
20,
21].
This study raises important points for public health planning, especially with regard to the distribution of resources and hospital training. The high concentration of care in a few hospitals indicates that strategies to decentralize and strengthen regional hospitals can relieve the pressure on large centers and facilitate access to treatment for patients in more remote areas. In addition, the data highlights the importance of facial trauma prevention policies, such as traffic safety and violence prevention awareness campaigns, which could help reduce the occurrence of facial fractures and, consequently, the demand for these treatments [
22].
Finally, information on the types of procedures, average length of hospital stay, and mortality rates provide information for improving clinical and safety protocols. Implementing evidence-based protocols and continuous training of health teams can improve the management of severe cases and reduce hospital stays, promoting more efficient and safe care. In summary, the data analyzed point to a growing demand for facial fracture care and the importance of strategic planning that takes into account both the strengthening of large centers and the expansion of regional capacity, ensuring a more equitable and effective health system in the treatment of facial trauma.
5. Conclusions
This study reveals a growing demand for treatment of facial fractures in Paraíba, with a high concentration of care in referral hospitals such as Dom Luiz Gonzaga Fernandes Hospital and Senador Humberto Lucena Hospital. This increase, coupled with factors such as traffic accidents and violence, indicates the need to strengthen the infrastructure of these centers and decentralize care to regional hospitals, improving access and reducing the overload on large centers. The low mortality rate is a positive point, but the differences in average hospital stays reflect the complexity of the cases and suggest improvements in efficiency. For an effective response, strategic planning that includes decentralization, strengthening of resources and preventive policies is essential. In this way, the health system will be able to meet the growing demand in an equitable and efficient manner, promoting the health and well-being of the population.
Author Contributions
Conceptualization, IHGS and MRMV; methodology: AJF, CCG and EAAZ.; formal analysis: PCSS and KDF; investigation: MEBH and FGCM; data curation: IHGS and EDR; writing—original draft preparation: IHGS, MRMV, AJF and CCG; writing—review & editing: PCSS, KDF, MEBH; visualization: FGCM; supervision, EDR; project administration: EDR and IHGS. All authors read and agreed to the published version of the manuscript.
Funding
This research did not receive funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study because the data for this study were taken from secondary data from the Brazilian Unified Health System (SUS).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the results of this research were taken from the DATASUS website of the Ministry of Health (Brazil). DATASUS provides information that can be used to support objective analyses of the health situation, evidence-based decision-making and the development of health action programs. Access was via the link:
https://datasus.saude.gov.br/informacoes-de-saude-tabnet/
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Roșu, A.-M.; Severin, F.; Roșu, O.C.; Cobzeanu, B.M.; Gherasimescu, S.; Sava, F.P.; Palade, D.O.; Drochioi, C.I.; Costan, V.V.; Cobzeanu, M.D. Patterns and Characteristics of Midface Fractures in North-Eastern Romania. Medicina 2023, 59, 510. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Kaur, T.; Kaur, J.; Kaur, Y.; Kapila, S.; Sandhu, A. Efficacy of Titanium Mesh Osteosynthesis in Maxillofacial Fractures. J. Maxillofac. Oral Surg. 2018, 17, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Sada-Urmeneta, A.; Tousidonis, M.; Navarro-Cuellar, C.; Ochandiano, S.; Navarro-Cuellar, I.; Khayat, S.; Ruiz-De-León, G.; Benito-Anguita, M.; Alvarez-Mokthari, S.; Olavarria, E.; et al. Dynamic Trends in Surgical Oromaxillofacial Trauma Epidemiology: A Comparative Study of Pre-COVID-19 and COVID-19 Periods in Tertiary Referral Hospitals in Madrid. J. Clin. Med. 2024, 13, 1947. [Google Scholar] [CrossRef]
- Kanta, M.K.; Kumar, S.R.; Harish, B.; Raja, A.T. Rare mandibular ramus fracture. Ann. Maxillofac. Surg. 2018, 8, 171–173. [Google Scholar] [CrossRef] [PubMed]
- Vigarani SZ, et al. Caracterização das guias de autorização de internação hospitalar (AIH) para cirurgias eletivas. CuidArte, Enferm, p. 251-256, 2020.
- Lima JS, et al. Custos das autorizações de internação hospitalar por quedas de idosos no Sistema Único de Saúde, Brasil, 2000-2020: um estudo descritivo. Epidemiologia e Serviços de Saúde, v. 31, n. 1, p. e2021603, 2022.
- Wusiman, P.D.; Maimaitituerxun, B.M.; Guli; Saimaiti, A. D.; Moming, A.D. Epidemiology and Pattern of Oral and Maxillofacial Trauma. J. Craniofacial Surg. 2020, 31, e517–e520. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.X.; Shah, N.; Gupta, A. Epidemiology of Nasal Bone Fractures. Facial Plast. Surg. Aesthetic Med. 2022, 24, 27–33. [Google Scholar] [CrossRef]
- Ahmad, W.M.A.W.; Noor, N.F.M.; Shaari, R.; Nawi, M.A.A.; Ghazali, F.M.M.; Aleng, N.A.; Rohim, R.A.A.; Alam, M.K. The Most Common Relationship of a Midface Fracture in Maxillofacial Trauma Study. J. Craniofacial Surg. 2021, 32, 1500–1503. [Google Scholar] [CrossRef] [PubMed]
- Estrela, Carlos. Metodologia científica: ciência, ensino, pesquisa. Artes médicas, 2018.
- Choi, S.H.; Gu, J.H.; Kang, D.H. Analysis of Traffic Accident-Related Facial Trauma. J. Craniofacial Surg. 2016, 27, 1682–1685. [Google Scholar] [CrossRef] [PubMed]
- Al-Hassani, A.; Ahmad, K.; El-Menyar, A.; Abutaka, A.; Mekkodathil, A.; Peralta, R.; Al Khalil, M.; Al-Thani, H. Prevalence and patterns of maxillofacial trauma: a retrospective descriptive study. Eur. J. Trauma Emerg. Surg. 2022, 48, 2513–2519. [Google Scholar] [CrossRef] [PubMed]
- Marsicano, J.A.; Cavalleri, N.Z.; Cordeiro, D.M.; Mori, G.G.; da Silveira, J.L.G.C.; Prado, R.L.D. Epidemiology of Maxillofacial Trauma in a Prehospital Service in Brazil. 2019, 26, 323–327. [CrossRef]
- Singh, A.K.; Dhungel, S.; Ahmad, Z.; Holmes, S. Can an App-Based Maxillofacial Trauma Score Predict the Operative Time, ICU Need and Length of Stay? Craniomaxillofacial Trauma Reconstr. 2022, 15, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Dhar, V.K.; Kim, Y.; Wima, K.; Hoehn, R.S.; Shah, S.A. The Importance of Safety-Net Hospitals in Emergency General Surgery. J. Gastrointest. Surg. 2018, 22, 2064–2071. [Google Scholar] [CrossRef]
- Botega, L.d.A.; Andrade, M.V.; Guedes, G.R. Profile of general hospitals in the Unified Health System. Rev. de Saude publica 2020, 54, 81–81. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.; Ellis, E. Complications of Mandibular Fracture Repair and Secondary Reconstruction. Semin. Plast. Surg. 2020, 34, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Chukwulebe, S.; Hogrefe, C. The Diagnosis and Management of Facial Bone Fractures. Emerg. Med. Clin. North Am. 2019, 37, 137–151. [Google Scholar] [CrossRef]
- Elzanie, A.S.; Park, K.E.B.; Irgebay, Z.B.; Choi, J.; Zellner, E.G. Zygoma Fractures Are Associated With Increased Morbidity and Mortality in the Pediatric Population. J. Craniofacial Surg. 2021, 32, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Sloane, D.M.; Brom, H.M.; Todd, B.A.D.; Barnes, H.; Cimiotti, J.P.; Cunningham, R.S.; McHugh, M.D.P. Value of Nurse Practitioner Inpatient Hospital Staffing. Med Care 2021, 59, 857–863. [Google Scholar] [CrossRef]
- Bosque-Mercader, L.; Siciliani, L. The association between bed occupancy rates and hospital quality in the English National Health Service. Eur. J. Heal. Econ. 2023, 24, 209–236. [Google Scholar] [CrossRef] [PubMed]
- Menon, C.S.; Mohan, A.R.; Nimmagadda, J.; Manohar, K.; Sham, M.E.; Archana, S.; Mathews, S.; Narayan, P.T. Incidence of Maxillofacial Injuries in the Emergency Department-Retrospective Study. J. Maxillofac. Oral Surg. 2024, 23, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).