Submitted:
04 December 2024
Posted:
05 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
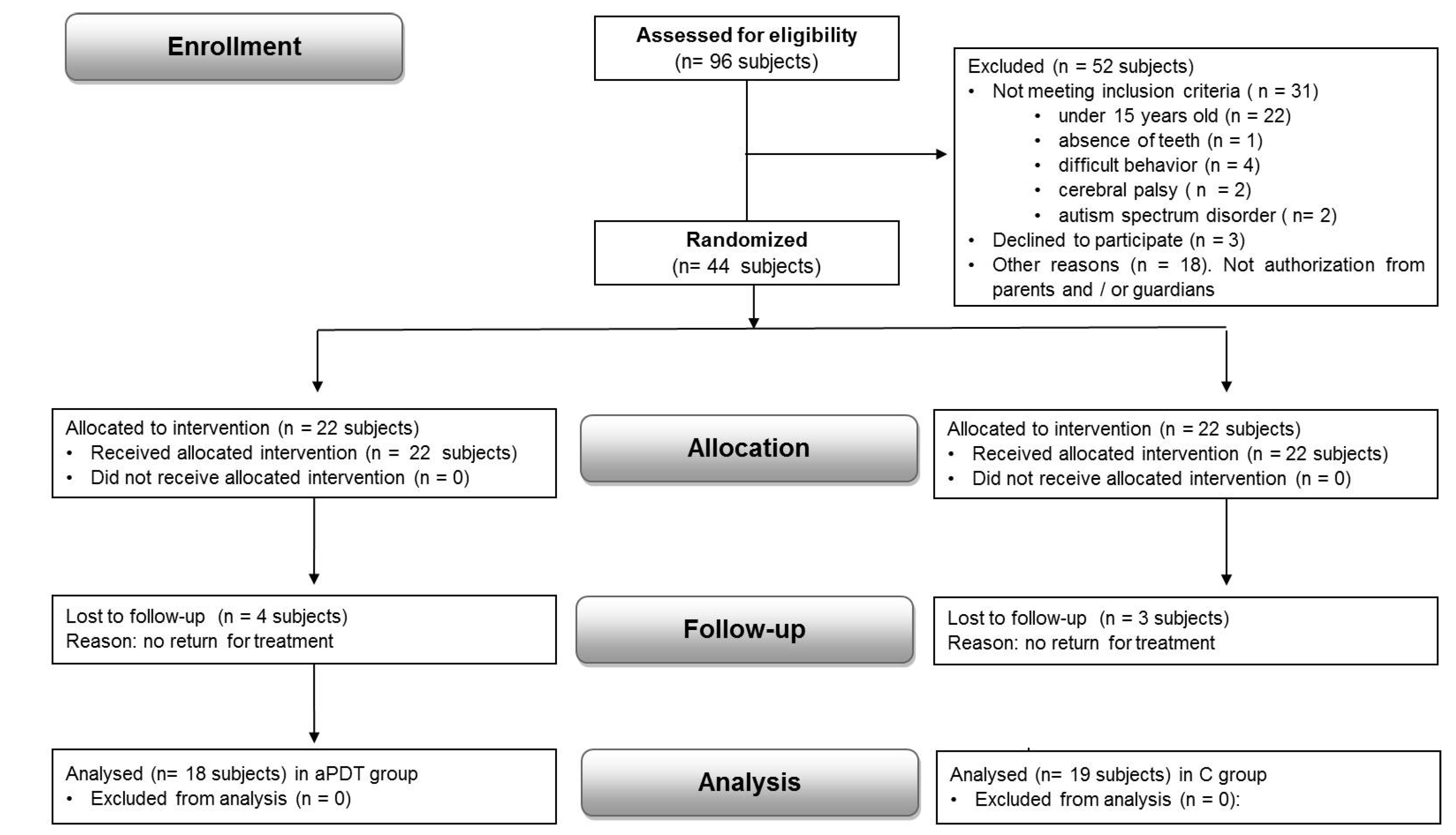
2.1. Sample Size Calculation
2.2. Inclusion and Exclusion Criteria
2.3. Clinical Parameters
2.4. Blinding
2.5. Randomization
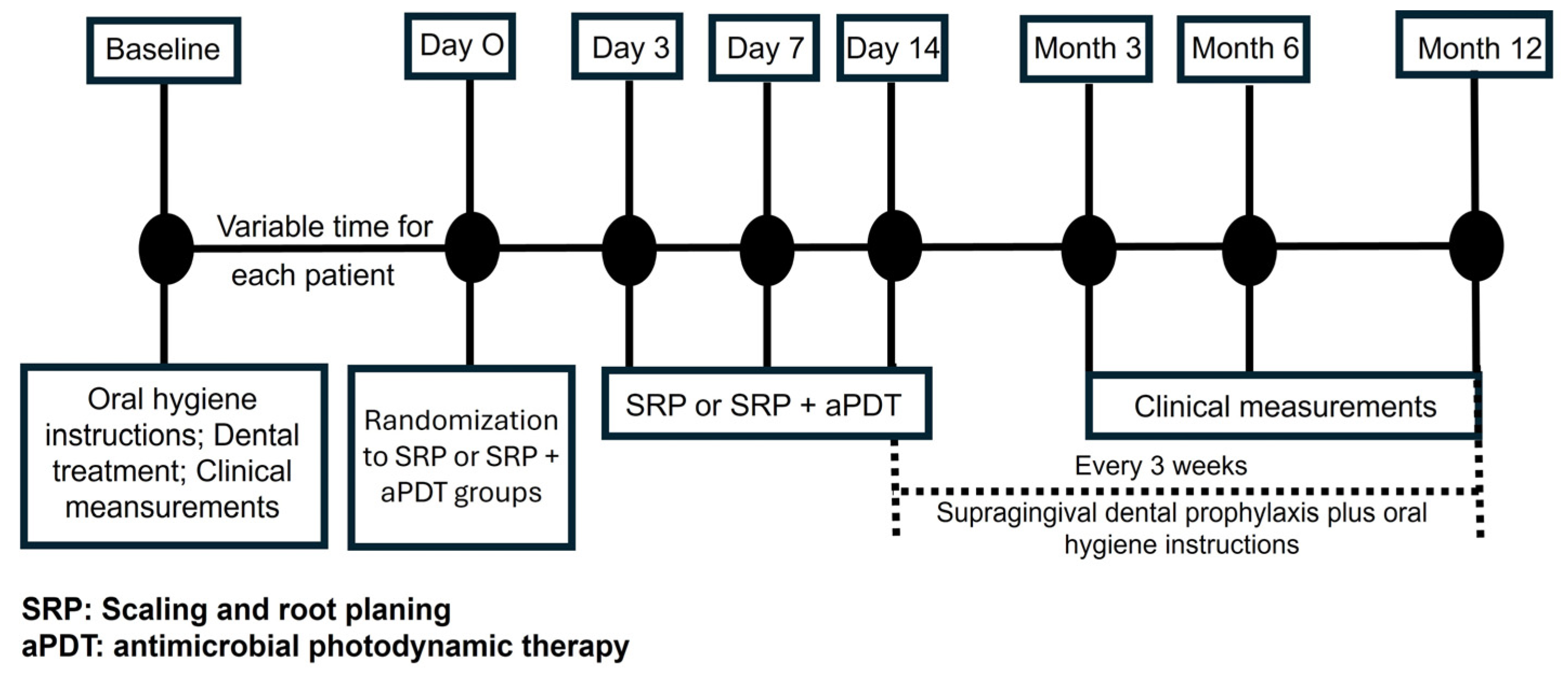
2.6. Study Design
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Belkady, B.; Elkhattabi, L.; Elkarhat, Z.; Zarouf, L.; Razoki, L.; Aboulfaraj, J.; Nassereddine, S.; Cadi, R.; Rouba, H.; Barakat, A. Chromosomal abnormalities in patients with intellectual disability: A 21-year retrospective study. Hum. Hered. 2018, 83, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Weijerman, M.E.; de Winter, J.P. Clinical practice. The care of children with Down syndrome. Eur. J. Pediatr. 2010, 169, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Scalioni, F.A.R.; Carrada, C.F.; Martins, C.C.; Ribeiro, R.A.; Paiva, S.M. Periodontal disease in patients with Down syndrome: A systematic review. J. Am. Dent. Assoc. 2018, 149, 628–639.e11. [Google Scholar] [CrossRef]
- Nuernberg, M.A.A.; Ivanaga, C.A.; Haas, A.N.; Aranega, A.M.; Casarin, R.C.V.; Caminaga, R.M.S.; Garcia, V.G.; Theodoro, L.H. Periodontal status of individuals with Down syndrome: Sociodemographic, behavioral, and family perception influence. J. Intellect. Disabil. Res. 2019, 63, 1181–1192. [Google Scholar] [CrossRef]
- Rondón-Avalo, S.; Rodríguez-Medina, C.; Botero, J.E. Association of Down syndrome with periodontal diseases: Systematic review and meta-analysis. Spec. Care Dentist. 2023, 44, 360–368. [Google Scholar] [CrossRef]
- Cutress, T.W. Periodontal disease and oral hygiene in trisomy 21. Arch. Oral Biol. 1971, 16, 1345–1355. [Google Scholar] [CrossRef]
- Desai, S.S. Down syndrome: A review of the literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997, 79, 279–285. [Google Scholar] [CrossRef]
- Fernández, M.; de Coo, A.; Quintela, I.; García, E.; Diniz-Freitas, M.; Limeres, J.; Diz, P.; Blanco, J.; Carracedo, Á.; Cruz, R. Genetic susceptibility to periodontal disease in Down syndrome: A case-control study. Int. J. Mol. Sci. 2021, 22, 6274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Otsuka, Y.; Ito, M.; Yamaguchi, M.; Saito, S.; Uesu, K.; Kasai, K. Enhancement of lipopolysaccharide-stimulated cyclooxygenase-2 mRNA expression and prostaglandin E2 production in gingival fibroblasts from individuals with Down syndrome. Mech. Ageing Dev. 2002, 123, 663–674. [Google Scholar] [CrossRef]
- Cavalcante, L.B.; Tanaka, M.H.; Pires, J.R.; Apponi, L.H.; Aparecida Giro, E.M.; Valentini, S.R. Expression of the interleukin-10 signaling pathway genes in individuals with Down syndrome and periodontitis. J. Periodontol. 2012, 83, 926–935. [Google Scholar] [CrossRef]
- Tsilingaridis, G.; Yucel-Lindberg, T.; Concha Quezada, H.; Modéer, T. The relationship between matrix metalloproteinases (MMP-3, -8, -9) in serum and peripheral lymphocytes (CD8+, CD56+) in Down syndrome children with gingivitis. J Periodontal Res. 2014, 49, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Domingues, N.B.; Mariusso, M.R.; Tanaka, M.H.; Scarel-Caminaga, R.M.; Mayer, M.P.A.; Brighenti, F.L.; Zuanon, Â.C.C.; Ibuki, F.K.; Nogueira, F.N.; Giro, E.M.A. Reduced salivary flow rate and high levels of oxidative stress in whole saliva of children with Down syndrome. Spec Care Dentist. 2017, 37, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Arul, D. Matrix Metalloproteinase Activity in Gingival Crevicular Fluid and Periodontal Health Status in Down Syndrome Patients: A Comparative Study. Cureus. 2023, 15, e40280. [Google Scholar] [CrossRef]
- Caton, G.J.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; et al. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018, 45, S1–S8. [Google Scholar] [CrossRef]
- Morinushi, T.; Lopatin, D.E.; Nakao, R.; Kinjyo, S. A comparison of the gingival health of children with Down syndrome to healthy children residing in an institution. Spec Care Dentist. 2006, 26, 13–19. [Google Scholar] [CrossRef]
- Martinez-Martinez, R.E.; Loyola-Rodriguez, J.P.; Bonilla-Garro, S.E.; Patiño-Marin, N.; Haubek, D.; Amano, A.; Poulsen, K. Characterization of periodontal biofilm in Down syndrome patients: a comparative study. J Clin Pediatr Dent. 2013, 37, 289–295. [Google Scholar] [CrossRef]
- Faria Carrada, C.; Almeida Ribeiro Scalioni, F.; Evangelista Cesar, D.; Lopes Devito, K.; Ribeiro, L.C.; Almeida Ribeiro, R. Salivary Periodontopathic Bacteria in Children and Adolescents with Down Syndrome. PLoS One. 2016, 11, e0162988. [Google Scholar] [CrossRef]
- Vocale, C.; Montevecchi, M.; D'Alessandro, G.; Gatto, M.; Piana, G.; Nibali, L.; Re, M.C.; Sambri, V. Subgingival periodontal pathogens in Down syndrome children without periodontal breakdown. A case-control study on deciduous teeth. Eur J Paediatr Dent. 2021, 22, 309–313. [Google Scholar]
- Mitsuhata, C.; Kado, N.; Hamada, M.; Nomura, R.; Kozai, K. Characterization of the unique oral microbiome of children with Down syndrome. Sci Rep. 2022, 12, 14150. [Google Scholar] [CrossRef]
- Tanaka, M.H.; Rodrigues, T.O.; Finoti, L.S.; Teixeira, S.R.; Mayer, M.P.; Scarel-Caminaga, R.M.; Giro, E.M. The effect of conventional mechanical periodontal treatment on red complex microorganisms and clinical parameters in Down syndrome periodontitis patients: a pilot study. Eur J Clin Microbiol Infect Dis. 2015, 34, 601–608. [Google Scholar] [CrossRef]
- Stabholz, A.; Shapira, J.; Shur, D.; Friedman, M.; Guberman, R.; Sela, M.N. Local application of sustained-release delivery system of chlorhexidine in Down’s syndrome population. Clin Prev Dent. 1991, 13, 9–14. [Google Scholar] [PubMed]
- Cheng, R.H.; Leung, W.K.; Corbet, E.F. Non-surgical periodontal therapy with adjunctive chlorhexidine use in adults with Down syndrome: a prospective case series. J Periodontol. 2008, 79, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Teitelbaum, A.P.; Pochapski, M.T.; Jansen, J.L.; Sabbagh-Haddad, A.; Santos, F.A.; Czlusniak, G.D. Evaluation of the mechanical and chemical control of dental biofilm in patients with Down syndrome. Community Dent Oral Epidemiol. 2009, 37, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Freedman, L.; Nunn, J.; Thomas, W.; Claffey, N.; Kelly, A. Preventive strategies to improve periodontal health in people with Down syndrome. J Disabil Oral Health. 2011, 12, 59–67. [Google Scholar]
- Zaldivar-Chiapa, R.M.; Arce-Mendoza, A.Y.; De La Rosa-Ramírez, M.; Caffesse, R.G.; Solis-Soto, J.M. Evaluation of Surgical and Non-Surgical Periodontal Therapies and Immunological Status of Young Down’s Syndrome Patients. J Periodontol. 2005, 76, 1061–1065. [Google Scholar] [CrossRef]
- Martins, F.; Simões, A.; Oliveira, M.; Luiz, A.C.; Gallottini, M.; Pannuti, C. Efficacy of antimicrobial photodynamic therapy as an adjuvant in periodontal treatment in Down syndrome patients. Lasers Med Sci. 2016, 31, 1977–1981. [Google Scholar] [CrossRef]
- Ferreira, R.; Michel, R.C.; Greghi, S.L.; Resende, M.L.; Sant'Ana, A.C.; Damante, C.A.; Zangrando, M.S. Prevention and Periodontal Treatment in Down Syndrome Patients: A Systematic Review. PLoS One. 2016, 11, e0158339. [Google Scholar] [CrossRef]
- Van Strydonck, D.A.; Slot, D.E.; Van der Velden, U.; Van der Weijden, F. Effect of a chlorhexidine mouthrinse on plaque, gingival inflammation and staining in gingivitis patients: a systematic review. J Clin Periodontol. 2012, 39, 1042–1055. [Google Scholar] [CrossRef]
- Kolbe, M.F.; Ribeiro, F.V.; Luchesi, V.H.; Casarin, R.C.; Sallum, E.A.; Nociti, F.H.; et al. Photodynamic therapy during supportive periodontal care: clinical, microbiologic, immunoinflammatory, and patient-centered performance in a split-mouth randomized clinical trial. J Periodontol. 2014, 85, e277–e286. [Google Scholar] [CrossRef]
- Luchesi, V.H.; Pimentel, S.P.; Kolbe, M.F.; Ribeiro, F.V.; Casarin, R.C.; Nociti, F.H.; et al. Photodynamic therapy in the treatment of class II furcation: a randomized controlled clinical trial. J Clin Periodontol. 2013, 40, 781–788. [Google Scholar] [CrossRef]
- Ge, L.; Shu, R.; Li, Y.; Li, C.; Luo, L.; Song, Z.; Xie, Y.; Liu, D. Adjunctive effect of photodynamic therapy to scaling and root planing in the treatment of chronic periodontitis. Photomed Laser Surg. 2011, 29, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Lui, J.; Corbet, E.F.; Jin, L. Combined photodynamic and low-level laser therapies as an adjunct to nonsurgical treatment of chronic periodontitis. J Periodontal Res. 2011, 46, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Giannelli, M.; Formigli, L.; Lorenzini, L.; Bani, D. Combined photoablative and photodynamic diode laser therapy as an adjunct to non-surgical periodontal treatment: a randomized split-mouth clinical trial. J Clin Periodontol. 2012, 39, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Franco, E.J.; Pogue, R.E.; Sakamoto, L.H.; Cavalcante, L.L.; Carvalho, D.R.; de Andrade, R.V. Increased expression of genes after periodontal treatment with photodynamic therapy. Photodiagnosis Photodyn Ther. 2014, 11, 41–47. [Google Scholar] [CrossRef]
- Betsy, J.; Prasanth, C.S.; Baiju, K.V.; Prasanthila, J.; Subhash, N. Efficacy of antimicrobial photodynamic therapy in the management of chronic periodontitis: a randomized controlled clinical trial. J Clin Periodontol. 2014, 41, 573–581. [Google Scholar] [CrossRef]
- Campanile, V.S.M.; Giannopoulou, C.; Campanile, G.; Cancela, J.A.; Mombelli, A. Single or repeated antimicrobial photodynamic therapy as adjunct to ultrasonic debridement in residual periodontal pockets: clinical, microbiological, and local biological effects. Lasers Med Sci. 2015, 30, 27–34. [Google Scholar] [CrossRef]
- Berakdar, M.; Callaway, A.; Eddin, M.F.; Ross, A.; Willershausen, B. Comparison between scaling-root-planing (SRP) and SRP/photodynamic therapy: six-month study. Head Face Med. 2012, 8, 12. [Google Scholar] [CrossRef]
- Noro Filho, G.A.; Casarin, R.C.; Casati, M.Z.; Giovani, E.M. PDT in non-surgical treatment of periodontitis in HIV patients: a split-mouth, randomized clinical trial. Lasers Surg Med. 2012, 44, 296–302. [Google Scholar] [CrossRef]
- Campos, G.N.; Pimentel, S.P.; Ribeiro, F.V.; Casarin, R.C.; Cirano, F.R.; Saraceni, C.H.; et al. The adjunctive effect of photodynamic therapy for residual pockets in single-rooted teeth: a randomized controlled clinical trial. Lasers Med Sci. 2013, 28, 317–324. [Google Scholar] [CrossRef]
- Andrade, P.F.; Garlet, G.P.; Silva, J.S.; Fernandes, P.G.; Milanezi, C.; Novaes, A.B. Jr.; et al. Adjunct effect of the antimicrobial photodynamic therapy to an association of non-surgical and surgical periodontal treatment in modulation of gene expression: a human study. J Photochem Photobiol B 2013, 126, 119–125. [Google Scholar] [CrossRef]
- Salvi, G.E.; Stähli, A.; Schmidt, J.C.; Ramseier, C.A.; Sculean, A.; Walter, C. Adjunctive laser or antimicrobial photodynamic therapy to non-surgical mechanical instrumentation in patients with untreated periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47 (Suppl 22), 176–198. [Google Scholar] [CrossRef] [PubMed]
- Chambrone, L.; Wang, H.L.; Romanos, G.E. Antimicrobial photodynamic therapy for the treatment of periodontitis and peri-implantitis: An American Academy of Periodontology best evidence review. J Periodontol. 2018, 89, 783–803. [Google Scholar] [CrossRef] [PubMed]
- Xue, D.; Tang, L.; Bai, Y.; Ding, Q.; Wang, P.; Zhao, Y. Clinical efficacy of photodynamic therapy adjunctive to scaling and root planing in the treatment of chronic periodontitis: A systematic review and meta-analysis. Photodiagnosis Photodyn Ther. 2017, 18, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Vohra, F.; Akram, Z.; Safi, S.H.; Devi Vaithilingam, R.; Ghanem, A.; Sergis, K.; Javed, F. Role of antimicrobial photodynamic therapy in the treatment of aggressive periodontitis: a systematic review. Photodiagnosis Photodyn Ther. 2015, 13, Epub. [Google Scholar] [CrossRef]
- Akram, Z.; Hyder, T.; Al-Hamoudi, N.; Binshabaib, M.S.; Alharthi, S.S.; Hanif, A. Efficacy of photodynamic therapy versus antibiotics as an adjunct to scaling and root planing in the treatment of periodontitis: A systematic review and meta-analysis. Photodiagnosis Photodyn Ther. 2017, 19, 86–92. [Google Scholar] [CrossRef]
- Xue, D.; Zhao, Y. Clinical effectiveness of adjunctive antimicrobial photodynamic therapy for residual pockets during supportive periodontal therapy: A systematic review and meta-analysis. Photodiagnosis Photodyn Ther. 2017, 17, 127–133. [Google Scholar] [CrossRef]
- Page, R.C.; Eke, P.I. Case definitions for use in population-based surveillance of periodontitis. J Periodontol. 2007, 78, 1387–1399. [Google Scholar] [CrossRef]
- Eke, P.I.; Thornton-Evans, G.; Dye, B.; Genco, R. Advances in surveillance of periodontitis: the Centers for Disease Control and Prevention Periodontal Disease Surveillance Project. J Periodontol. 2012, 83, 1337–1342. [Google Scholar] [CrossRef]
- Ainamo, J.; Bay, I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975, 25, 229–235. [Google Scholar]
- Dilsiz, A.; Canakci, V.; Aydin, T. Clinical effects of potassium-titanyl-phosphate laser and photodynamic therapy on outcomes of treatment of chronic periodontitis: a randomized controlled clinical trial. J Periodontol. 2013, 84, 278–286. [Google Scholar] [CrossRef]
- Lulic, M.; Leiggener, G.; Salvi, G.E.; Ramseier, C.A.; Mattheos, N.; Lang, N.P. One-year outcomes of repeated adjunctive photodynamic therapy during periodontal maintenance: a proof-of-principle randomized-controlled clinical trial. J Clin Periodontol. 2009, 36, 661–666. [Google Scholar] [CrossRef] [PubMed]
- Alwaeli, H.A.; Al-Khateeb, S.N.; Al-Sadi, A. Long-term clinical effect of adjunctive antimicrobial photodynamic therapy in periodontal treatment: a randomized clinical trial. Lasers Med Sci. 2015, 30, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Goh, E.X.; Tan, K.S.; Chan, Y.H.; Lim, L.P. Effects of root debridement and adjunctive photodynamic therapy in residual pockets of patients on supportive periodontal therapy: A randomized split-mouth trial. Photodiagnosis Photodyn Ther. 2017, 18, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Sgolastra, F.; Petrucci, A.; Gatto, R.; Marzo, G.; Monaco, A. Photodynamic therapy in the treatment of chronic periodontitis: a systematic review and meta-analysis. Lasers Med Sci. 2013, 28, 669–682. [Google Scholar] [CrossRef] [PubMed]
- Azaripour, A.; Dittrich, S.; Van Noorden, C.J.F.; Willershausen, B. Efficacy of photodynamic therapy as adjunct treatment of chronic periodontitis: a systematic review and meta-analysis. Lasers Med Sci. 2018, 33, 33–407. [Google Scholar] [CrossRef]
- Almeida, J.M.; Theodoro, L.H.; Bosco, A.F.; Nagata, M.J.; Bonfante, S.; Garcia, V.G. Treatment of experimental periodontal disease by photodynamic therapy in rats with diabetes. J Periodontol. 2008, 79, 2156–2165. [Google Scholar] [CrossRef]
- Prates, R.A.; Yamada, A.M.; Suzuki, L.C.; França, C.M.; Cai, S.; Mayer, M.P.; et al. Histomorphometric and microbiological assessment of photodynamic therapy as an adjuvant treatment for periodontitis: a short-term evaluation of inflammatory periodontal conditions and bacterial reduction in a rat model. Photomed Laser Surg. 2011, 29, 835–844. [Google Scholar] [CrossRef]
- Moreira, A.L.; Novaes, A.B. Jr.; Grisi, M.F.; Taba, M.Jr.; Souza, S.L.; Palioto, D.B.; et al. Antimicrobial Photodynamic Therapy as an Adjunct to Nonsurgical Treatment of Aggressive Periodontitis: a Split-mouth Randomized Controlled Trial. J Periodontol. 2015, 86, 376–386. [Google Scholar] [CrossRef]
- Franco, T.P.M.; Dos Santos, A.P.P.; Canabarro, A. The effects of repeated applications of antimicrobial photodynamic therapy in the treatment of residual periodontal pockets: a systematic review. Lasers Med Sci. 2019, 34, 855–863. [Google Scholar] [CrossRef]
- Shyama, M.; Al-Mutawa, S.A.; Honkala, S.; Honkala, E. Supervised toothbrushing and oral health education program in Kuwait for children and young adults with Down syndrome. Spec Care Dent. 2003, 23, 94–99. [Google Scholar] [CrossRef]
| Group | Mean age (years) | Sex | Ethnicity | Number of evaluated teeth (n) | ||
|---|---|---|---|---|---|---|
| Male (%) | Female (%) | White (%) | Black (%) | |||
| aPDT | 29.44±7.82 | 7(38.9%) | 11(61.1%) | 11(61.1%) | 7(78.9%) | 23.89±5.75 |
| C | 27.21±6.92 | 8(42.1%) | 11(57.9%) | 13(68.4%) | 6(31.6%) | 23.11±6.17 |
| Total | 28.42±7.41 | 15(40.5%) | 22 (59.5%) | 24(65%) | 13(35%) | 23.7±6.02 |
| Periodontal parameters | Groups | Baseline | 3 months | 6 months | 12 months |
|---|---|---|---|---|---|
|
PD (mm) |
aPDT | 4.01 ± 0.96aA | 2.57 ± 0.91bA | 2.62 ± 0.89bA | 2.54 ± 0.73bA |
| C | 4.16 ± 0.93aA | 2.49 ± 0.61bA | 2.59 ± 0.54bA | 2.47 ± 0.75bA | |
|
CAL (mm) |
aPDT | 6.72 ± 0.65 aA | 4.58 ± 0.54bA | 4.65 ± 0.55bA | 4.59 ± 0.56bA |
| C | 6.84 ± 0.55 aA | 4.72 ± 0.44bB | 4.74 ± 0.43bA | 4.84 ± 0.51bB | |
|
BOP (% sites) |
aPDT | 57.35 ± 19.41aA | 29.87 ± 11.66bA | 36.82 ± 5.78cA | 38.37 ± 15.74cA |
| C | 51.48 ± 19.17aA | 34.63 ± 13.59bA | 41.1 ± 15.27cA | 36.09 ± 16.24cA | |
|
PI (% sites) |
aPDT | 85.67 ± 1.74aA | 63.94 ± 3.11bA | 74.33 ± 2.37cA | 67.89 ± 6.32cA |
| C | 86.53 ± 1.64aA | 65.37 ± 3.04bA | 72.89 ± 2.96cA | 69.74 ± 4.94cA |
| Probing depth range | Group | Baseline | 3 months | 6 months | 12 months |
|---|---|---|---|---|---|
| 1-3mm | aPDT | 136.83 ± 28.4aA | 147.39 ± 21.5bA | 147.39 ± 27.5bA | 146.83 ± 21.4bA |
| C | 113.68 ± 45.1aA | 121.68 ± 39bB | 118.68 ± 36bB | 121.5 ± 38.8bB | |
| 4-5mm | aPDT | 15.94 ± 10.6aA | 6.33 ± 10.6aA | 6.33 ± 10.6aA | 7.39 ± 11.5aA |
| C | 20.26 ± 12.1aA | 10.4 ± 10.5aA | 12 ± 10.7aA | 11.47 ± 11.4aA | |
| 6-7mm | aPDT | 1.78 ± 2.5aA | 0.56 ± 1.3 aA | 0.61 ± 1.5aA | 0.61 ± 1.5aA |
| C | 2.63 ± 3.2aA | 0.95 ± 2 aA | 1.05 ± 2.3aA | 1.05 ± 2.3aA | |
| >7mm | aPDT | 0.17 ± 0.3aA | 0 ± 0aA | 0 ± 0aA | 0 ± 0aA |
| C | 0.42 ± 0.6aA | 0 ± 0aA | 0 ± 0aA | 0 ± 0aA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





