1. Introduction
Despite the development of many alternative methods for management of aortic regurgitation (AR), the gold standard for treatment remains aortic valve replacement (AVR) with mechanical or biological valves. As recent guidelines also expanded the indications for surgery for AR [
1,
2,
3], the application of surgical treatment for AR is expected to increase in the future. In AVR, the differences in durability between biological and mechanical valves according to age [
4] or valve-related events due to anticoagulation therapy have long been a matter of debate [
5,
6].
Valve-sparing aortic root replacement (VSRR) is one surgical option for aortic root enlargement with or without AR. Valve-sparing operations for tricuspid and bicuspid valves have yielded excellent results [
7,
8,
9] and it is advantageous to resolve the concerns of anticoagulation and durability associated with mechanical and biological valves, respectively. Nonetheless, as limited durability of biological valves can be solved by transcatheter aortic valve implantation in surgical AVR, VSRR should provide more durability for widespread application. Evaluation of the mechanisms of AR and morphology of the aortic root are crucial to determine the feasibility and success of VSRR. Schäfers et al. proposed tricuspid aortic valve (TAV) and bicuspid aortic valve (BAV) geometric heights (GHs) of 16 mm and 19 mm, respectively, as cutoff values for performing valve-sparing surgery [
10]. However, as they were derived from intraoperative data, they were difficult to predict before surgery. The aortic valve leaflet motion is difficult to assess with transthoracic echocardiography (TTE), and contrast-enhanced computed tomography (CT) is associated with concerns about the risks of radiation exposure.
The present study was performed to determine the suitability of VSRR for patients with AR preoperatively using three-dimensional transesophageal echocardiography (3D-TEE).
2. Materials and Method
2.1. Patient Selection and Surgical Methods
A total of 124 patients undergoing elective aortic root replacement surgery between September 2014 and March 2019 were enrolled in this study. Patients with infective endocarditis, acute aortic dissection, history of previous cardiac surgery, unicuspid or quadricuspid aortic valve, AR due to rheumatic changes, relevant aortic stenosis, age over 70 years, or who did not undergo preoperative TEE were excluded. Patients who underwent concomitant cardiac surgery were not excluded. Application of VSSR or root replacement using composite valve graft (Bentall operation) was decided by the surgeon intraoperatively, and patients were divided into either the VSRR or Bentall group. All operations were performed with median full sternotomy. If circulatory arrest was necessary, the core temperature was cooled to 25°C and retrograde cerebral perfusion was used. VSRR was performed by aortic root remodeling with external flexible ring annuloplasty as described previously by Lansac et al. [
11]. Briefly, all three sinuses of Valsalva were replaced using either a neo-Valsalva graft (Gelweave Valsalva; Terumo, Tokyo, Japan) or a tube graft (J Graft; Japan Lifeline, Tokyo, Japan) with three tongue-shaped incisions matching their shape. External flexible ring annuloplasty was performed using the same graft cut into 5 mm pieces, which were fixed at the basal ring level with 6 pledgeted mattress sutures (Tefdesser; Crownjun, Chiba, Japan). Bentall operation was performed using a handmade composite valve graft with either mechanical or biological prosthesis. Coronary arteries were reconstructed with the Carrel patch technique in all cases. Comparisons were performed based on preoperative 3D-TEE parameters, aortoventricular junction (AVJ), GH, diameters of the sinus of Valsalva and sinotubular junction (STJ), and long-term outcomes with an average follow-up of 43 ± 20 months. The follow-up duration was significantly different between the two groups: VSRR group, 46 ± 19 months; Bentall group, 33 ± 20 months (P < .01). The institutional review boards of both participating institutions approved this study (approval numbers: 32-076 (10151) and 19-086). The requirement for written informed consent was waived due to the retrospective nature of the study.
2.2. Statistical Analysis
Statistical analyses were performed using SPSS ver. 28 (SPSS Inc., Chicago, IL, USA). Normally distributed continuous variables are expressed as the mean ± standard deviation, and nonnormally distributed continuous variables are expressed as the median with interquartile range. Student’s t test or Wilcoxon’s signed rank test was used for comparison of continuous variables between the two groups, as appropriate. Categorical variables are expressed as number and percentage and were compared between the two groups using the Chi-square test. Survival rate and reintervention-free rate were calculated using the Kaplan-Meier method and compared with the log-rank test. In all analyses, P < .05 was taken to indicate statistical significance.
3. Results
3.1. Preoperative Data
The preoperative characteristics are summarized in
Table 1. The VSRR group was significantly younger (50 ± 13 years vs. 59 ± 10 years, respectively,
P < .01) and had significantly better left ventricular ejection fraction (55.4% ± 8.0% vs. 50.9% ± 9.3%, respectively,
P = .01) than the Bentall group. Compared to the VSRR group, the Bentall group included more women (10.3% vs. 22.2%, respectively,
P = .11) and more patients with atrial fibrillation (2.1% vs. 11.1%, respectively,
P = .07), but the differences were not significant. BAV was observed in approximately one third of patients in both groups (34.0% and 29.7%, respectively,
P = .67).
In 3D-TEE measurement, there were no significant differences in AVJ area, diameter of the sinus of Valsalva, or STJ diameter between the groups (
Table 2). Only GH was significantly longer in the tricuspid aortic valve of the VSRR group compared to the Bentall group (
Table 3 and
Table 4).
3.2. Operative Data
Operative data is shown in
Table 5. Cardiopulmonary bypass time (226 ± 46 min vs. 191 ± 63 min, respectively,
P < .01) and aortic cross-clamp time (184 ± 38 min vs. 151 ± 52 min, respectively,
P < .01) were significantly longer in the VSRR group than the Bentall group. For VSRR, central plication was performed in the majority of patients and autologous pericardium was used in one third of the patients.
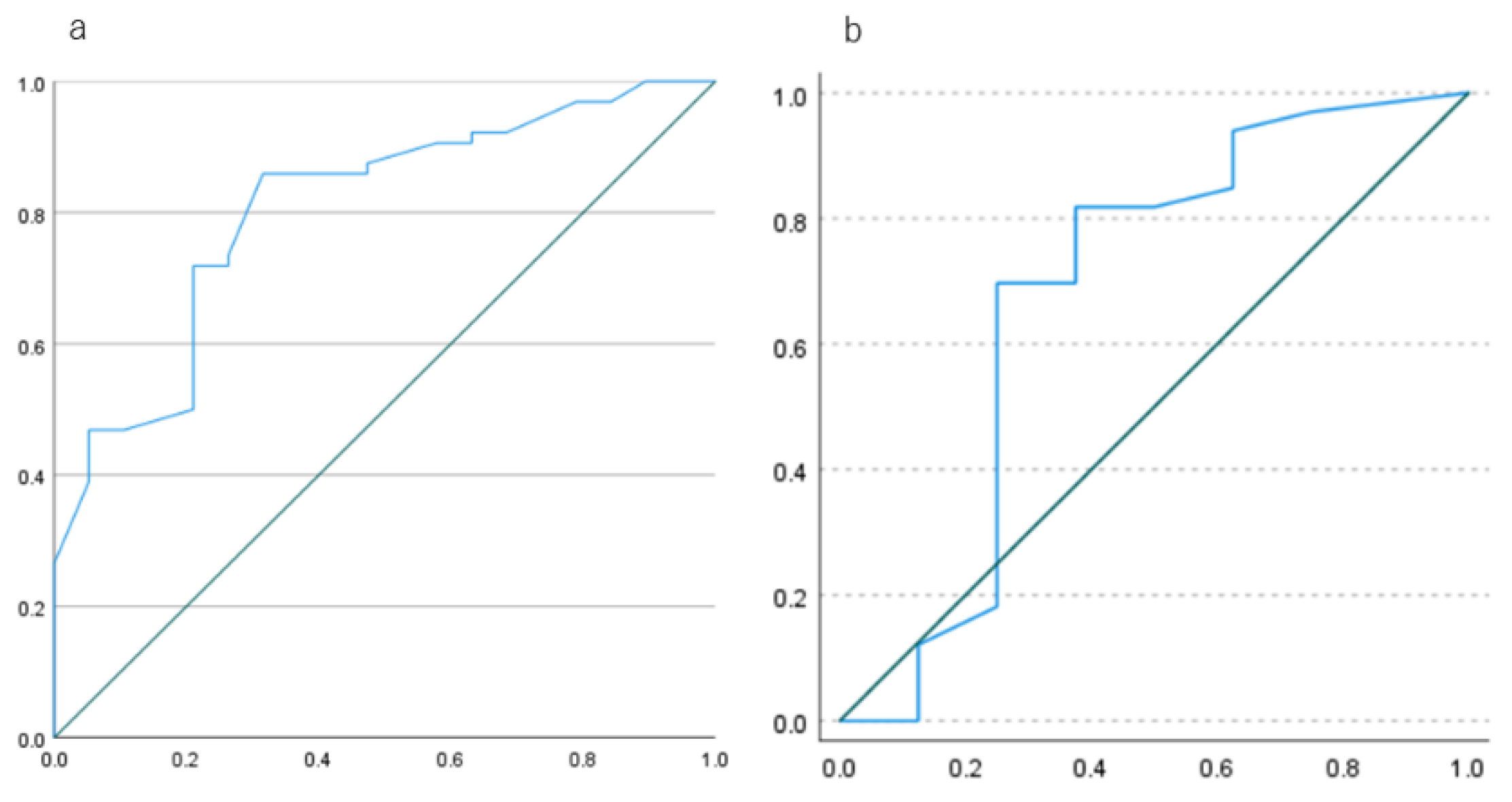
In receiver-operating curve (ROC) analysis, the optimal cutoff values of GH for detecting the suitability of VSRR were 15.9 mm in TAV and 19.8 mm in BAV (
Figure 1).
3.2. Postoperative Data
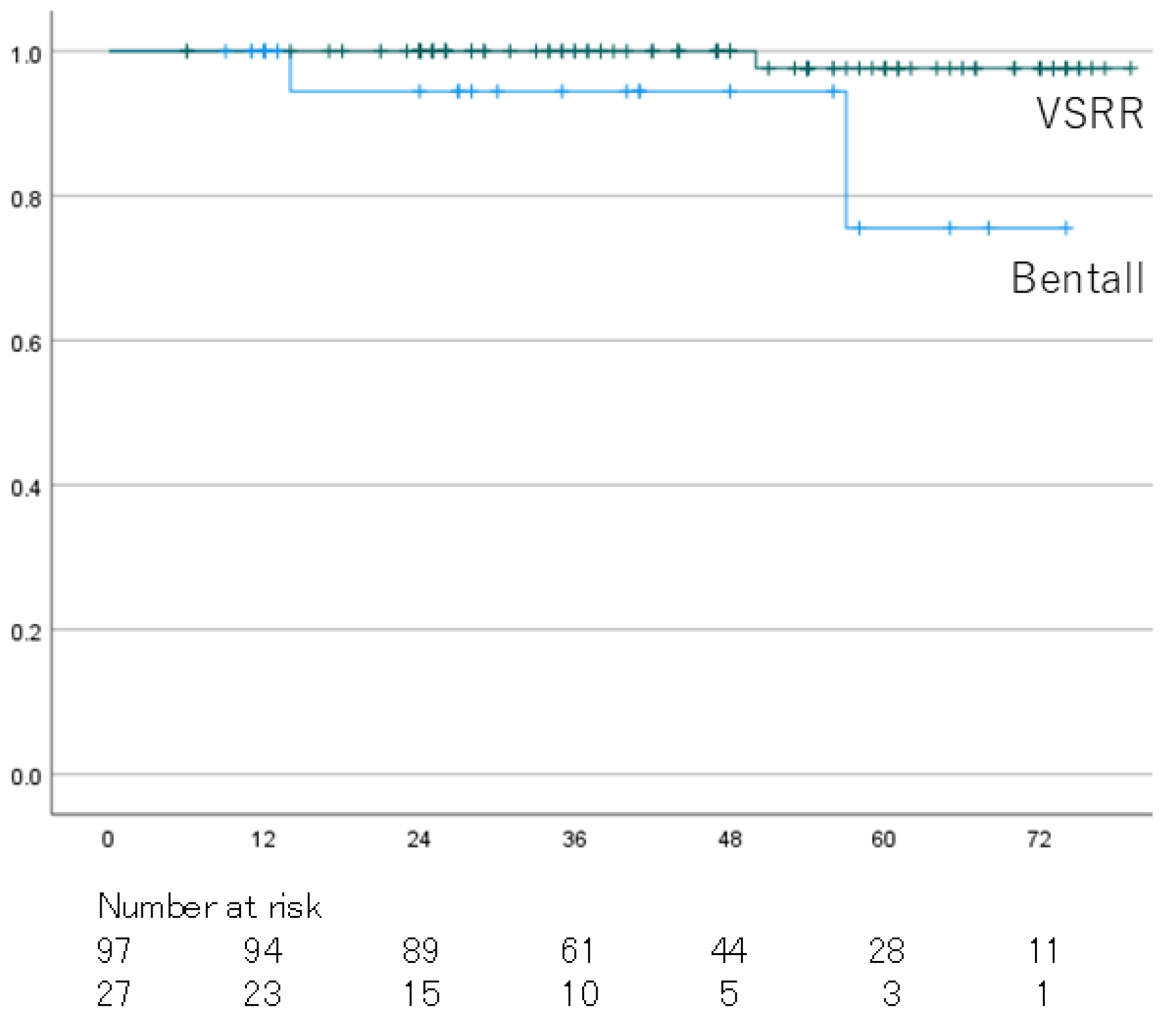
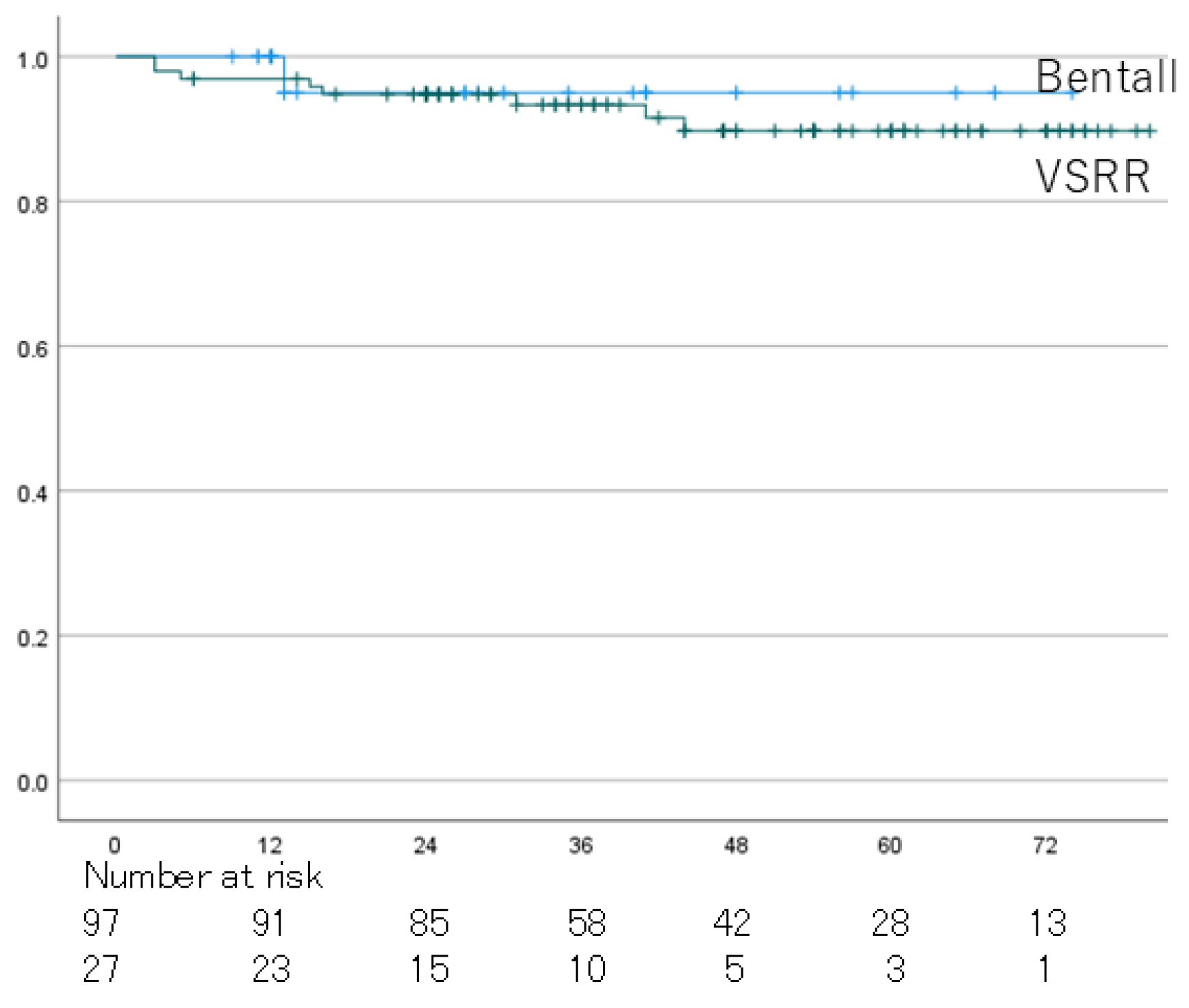
Overall survival rates at 5 years were 97.6% in the VSRR group and 75.6% in the Bentall group (P < .01) (
Figure 2). The reoperation-free rates at 5 years were 89.7% in the VSSR group and 95.0% in the Bentall group, and the difference was not significant (P = .63) (
Figure 3).
4. Discussion
AVR with biological or mechanical valves has been the gold standard surgical treatment for AR. In groups matched for age and sex, overall survival after AVR was reported to be the same as in the general population [
12]. In a meta-analysis comparing AVP and AVR, in-hospital mortality and long-term event rates were lower in AVP than AVR [
13]. Although use of a biological prosthesis requires no anticoagulation therapy, it is associated with a risk of structural valve deterioration or prosthesis/patient mismatch. Younger patients with biological valves have a lower survival rate than the general population, despite the low risk of reoperation [
14]. In addition, use of a mechanical valve is a risk factor for bleeding and thromboembolic events due to anticoagulation therapy, with a significant impact on survival [
15].
VSRR is one of the surgical options for aortic root enlargement with or without AR. Recent studies have demonstrated good late results of VSRR for patients with annuloaortic ectasia, BAV, and isolated AR [
8,
9,
16].
The valve-in-valve procedure (transcatheter AVR in surgical AVR) has been performed in recent years, but the late outcomes are unclear. The durability of biological prostheses has improved, so that valve-sparing surgery should also provide longer durability and become more widely adopted.
Schäfers et al. proposed that cusp height is one of the most important parameters for performing valve-sparing surgery. They stated that the method of measurement of GH is important and that it was underestimated in previous methods [
10].
In this study, the VSSR group was significantly younger and had better left ventricular function but required longer procedure times than the Bentall group. These differences may have been due to surgeon-dependent decisions on the procedure with the assignment of high-risk patients, such as those of advanced age or with low cardiac function, to the Bentall group. In other studies, procedure time was also significantly longer in the VSRR group, which was a natural result considering the complexity of the procedure [
17,
18].
We used 3D-TEE in this study. TEE allows more detailed evaluation of leaflet motion and root structure than TTE, and 3D-TTE allows accurate evaluation of GH. In this study, there were no differences in diameter of AVJ, sinus of Valsalva, and STJ, so there were also no differences in surgical indications for aortic root replacement between the two groups. Only GH was significantly longer in TAV in the VSRR group, but there was no difference in BAV. This may have been due to the small number of cases with BAV. When the leaflet motion and GH are adequate, root replacement with a prosthesis of appropriate size is important for the success of VSRR. In ROC analysis, the optimal GH cutoff values for determining suitability for VSRR were 15.9 mm in TAV and 19.8 mm in BAV, which were close to the values proposed by Schäfers et al. [
10].
There was a significant difference in long-term survival rate between the two groups, which was likely due to the age difference between the two groups. The 5-year survival rate of the VSRR group was 97.6% ± 2.6%, which was similar to previous studies [
17,
18]. There was no difference in the reoperation-free rate between the two groups. The 5-year reoperation-free rate of the VSRR group was 89.7% ± 3.6%, which was slightly lower than in previous studies [
17,
18]. This may have been due to the use of autologous pericardium in 35.1% of the cases in this study. In our study, differences in preoperative background were associated with differences in long-term survival. In other studies that included propensity score matching, long-term survival and reintervention rate were better for VSRR than Bentall operation with biological valves [
19].
Appropriate patient selection and adequate GH may contribute to the success of VSSR and improve long-term outcomes.
5. Conclusions
It is important to measure the geometry of the aortic root using an appropriate method to ensure acceptable long-term durability after valve-preserving surgery.
6. Limitations
This study had several limitations. The sample size was small, and this was a retrospective and nonrandomized study, so considerable inhomogeneity between the two groups remained a matter of concern. It would be ideal to perform matching between the groups, but this would have further reduced the sample size. The choice of surgery was left to the surgeon’s decision, and there were no selection criteria for determining which procedure to perform. The follow-up period was also relatively short, so long-term outcomes should be analyzed in future studies. Nonetheless, the detailed evaluation of the aortic root geometry in this study will contribute to the further success and widespread adoption of valve-preserving surgery.
Author Contributions
S.T. and T.S.; Conceptualization, S.Y. and T.K.; methodology, S.Y.; formal analysis, S.Y.; investigation, S.Y.; data curation, S.Y.; writing—original draft preparation, T.K.; writing—review and editing, T.K.; supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The institutional review boards of both participating institutions approved this study (approval numbers: 32-076 (10151) and 19-086).
Informed Consent Statement
The requirement for written informed consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data that support the findings will be made available on request by the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Catherine, M. Otto, MD, Rick A. Nishimura, MD, Robert O. Bonow, MD, MS et al. Circulation. 2021;143:e72–e227.
- 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Friedhelm Beyersdorf, Alec Vahanian, Milan Milojevic et al. 2021.
- JCS/JSCS/JATS/JSVS 2020 Guidelines on the Management of Valvular Heart Disease. Chisato Izumi, Kiyoyuki Eishi, Kyomi Ashihara et al. 2020.
- Andrew B Goldstone, Peter Chiu, Michael Baiocchi et al. Mechanical or Biologic Prostheses for Aortic-Valve and Mitral-Valve Replacement. N Engl J Med. 2017;377:1847-1857.
- A G Turpie, MD. Safer anticoagulant therapy after heart valve replacement. Postgrad Medicine 997;101:85-6, 89-90, 93-4.
- Tarun Chakravarty, Lars Søndergaard, John Friedman et al. Subclinical leaflet thrombosis in surgical and transcatheter bioprosthetic aortic valves: an observational study. Lancet. 2017.
- Hans-Joachim Schäfers, MD, Alexander Raddatz, MD, Wolfgang Schmied et al. Reexamining remodeling. S: 2015;149, 2015.
- Saadallah Tamer, MD, Stefano Mastrobuoni, MD, David Vancraeynest et al. Late results of aortic valve repair for isolated severe aortic regurgitation. J Thorac Cardiovasc Surg. 2023;165:995-1006.
- Tristan Ehrlich, Karen B Abeln, Lennart Froede et al. Twenty-five years' experience with isolated bicuspid aortic valve repair: impact of commissural orientation. Eur J Cardiothorac Surg. 2024;65:ezae163.
- Hans-Joachim Schäfers, Wolfram Schmied, Gil Marom, Diana Aicher. Cusp height in aortic valves. J Thorac Cardiovasc Surg. 2: 2013;146, 2013.
- Emmanuel Lansac, Isabelle Di Centa, Jan Vojacek et al. Valve sparing root replacement: the remodeling technique with external ring annuloplasty. 1: Ann Cardiothorac Surg 2013;2(1), 2013.
- Ismail Bouhout, Louis-Mathieu Stevens, Amine Mazine et al. Long-term outcomes after elective isolated mechanical aortic valve replacement in young adults. J Thorac Cardiovasc Surg. 2014;148:1341-1346.
- Chris Ho Ming Wong, Jeffrey Shi Kai Chan, Dilan Sanli et al. Aortic valve repair or replacement in patients with aortic regurgitation: A systematic review and meta-analysis. J Card Surg. 2019;34:377-384.
- Jessica Forcillo, Ismail El Hamamsy, Louis-Mathieu Stevens et al. The perimount valve in the aortic position: twenty-year experience with patients under 60 years old. Ann Thorac Surg. 2014;97:1526-32.
- Diana Aicher, Annika Holz, Susanne Feldner et al. Quality of life after aortic valve surgery: replacement versus reconstruction. J Thorac Cardiovasc Surg. 2011;142:e19-24.
- Emmanuel Lansac, Isabelle Di Centa, Ghassan Sleilaty et al. Remodeling root repair with an external aortic ring annuloplasty. J Thorac Cardiovasc Surg. 2017;153:1033-1042.
- Casidhe-Nicole Bethancourt, BA, David Blitzer, Tsuyoshi Yamabe et al. Valve-Sparing Root Replacement Versus Bio-Bentall: Inverse Propensity Weighting of 796 Patients. 1: Ann Thorac Surg 2022;113, 2022.
- Elizabeth, L. Nortona, Parth M. Patela, Dov Levine et al. Bentall versus valve-sparing aortic root replacement for root pathology with moderate-to-severe aortic insufficiency: a propensity-matched analysis. 2023. [Google Scholar]
- Dov Levine, Parth Patel, Chunhui Wang et al. Valve-sparing root replacement versus composite valve graft root replacement: Analysis of more than 1500 patients from 2 aortic centers.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).