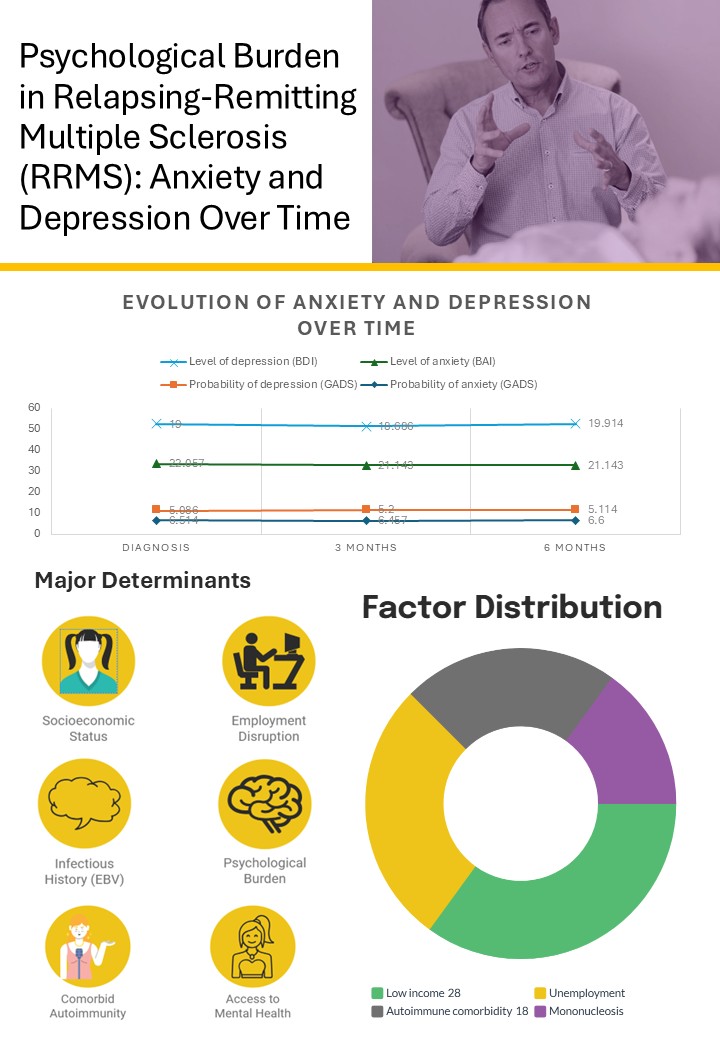
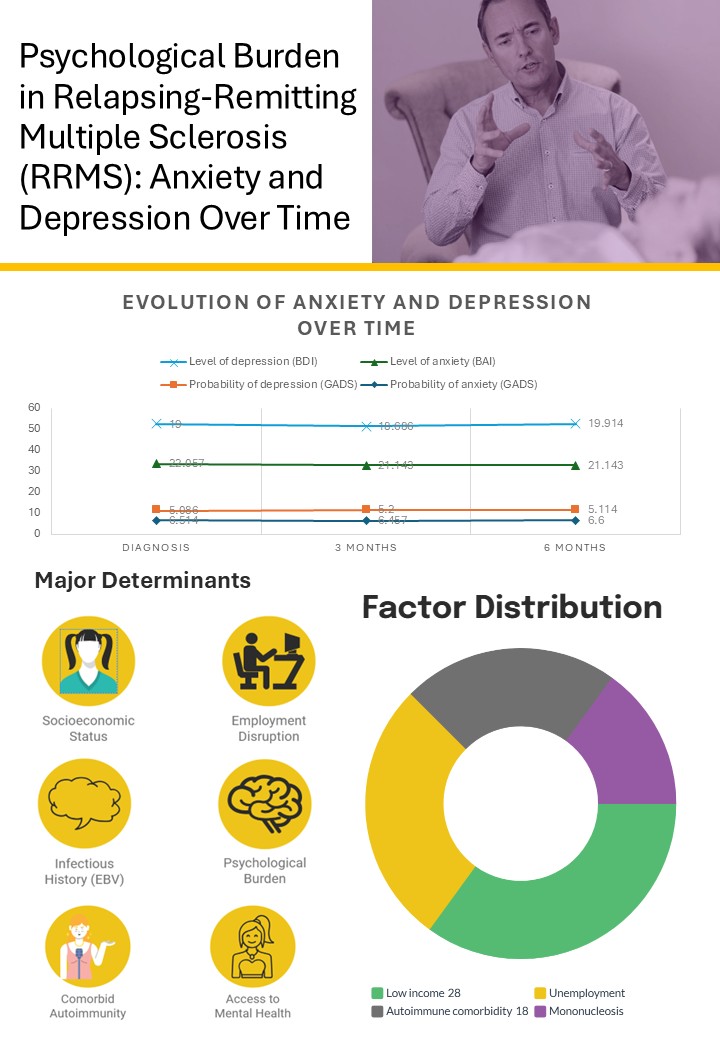
Background/Objectives: Multiple sclerosis (MS) is a chronic neurological disease characterized by demyelination, inflammation, and autoimmunity, leading to progressive physical and psychological impairments. Anxiety and depression are among the most prevalent neuropsychiatric comorbidities in MS, significantly impacting patients’ quality of life (QoL). This study aimed to assess the evolution of anxiety and depression in individuals with relapsing-remitting multiple sclerosis (RRMS) over a six-month follow-up period, identify associated factors, and explore predictive variables. Methods: A prospective observational study was conducted with 35 RRMS patients diagnosed at the Lucus Augusti University Hospital between January 2023 and March 2025. Psychological symptoms were assessed at baseline, 3 months, and 6 months using Goldberg Anxiety and Depression Scale (GADS), the Beck Depression Inventory (BDI), and the Beck Anxiety Inventory (BAI). Data were analyzed using non-parametric and parametric tests to account for the small sample size and distribution of variables. Results: Anxiety and depression were prevalent and persistent in the study population, with no significant changes in mean scores over time (p > 0.05). However, specific symptoms, such as pessimism and loss of pleasure, showed worsening trends, while sadness and guilt remained stable. Sociodemographic factors, including lower income and employment status, were significantly associated with higher anxiety and depression scores (p < 0.05). Additionally, clinical factors such as autoimmune comorbidities and a history of mononucleosis were linked to higher depressive symptoms. Baseline anxiety and depression scores emerged as strong predictors of future levels (p < 0.01), emphasizing the importance of early assessments. Conclusions: Anxiety and depression are prevalent and persistent in RRMS patients, with specific symptoms fluctuating over time. Sociodemographic and clinical factors play a significant role in psychological outcomes, highlighting the need for integrated care models that address both physical and psychosocial aspects of MS. Early psychological assessments and targeted interventions are critical to improving QoL and mitigating the long-term burden of mental health challenges in RRMS.